Report on 2026 Health Insurance Premium Increases and Implications for Sustainable Development Goals
Introduction: Challenges to SDG 3 (Good Health and Well-being)
A review of preliminary 2026 rate filings from health insurers indicates a significant rise in premiums, posing a direct challenge to the principles of Sustainable Development Goal 3 (Good Health and Well-being), particularly Target 3.8, which aims to achieve universal health coverage and financial risk protection. An analysis of 105 insurers across 19 states and the District of Columbia reveals a median premium increase of 15%. This escalation is driven by a combination of rising healthcare costs, policy changes, and economic factors that threaten the affordability and accessibility of healthcare for many Americans.
Primary Drivers of Premium Increases and Their Impact on SDGs
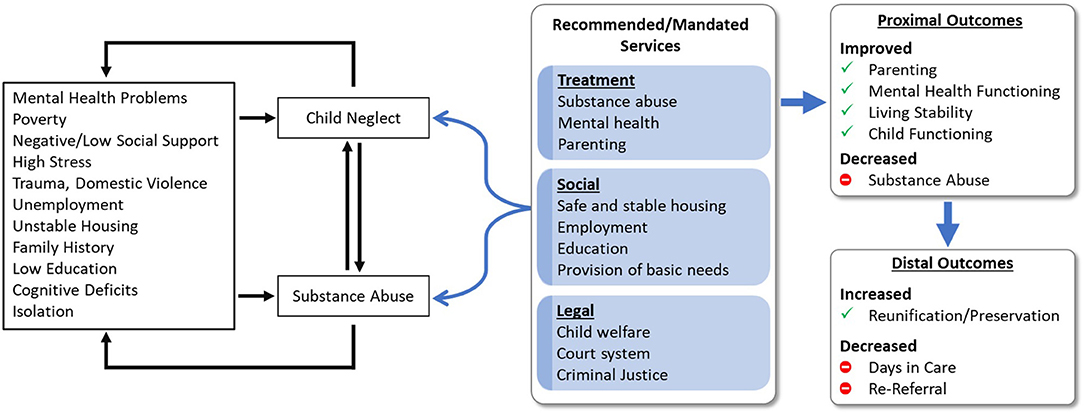
Several key factors are cited by insurers as drivers for the proposed rate hikes. Each of these factors has direct implications for progress on the Sustainable Development Goals, primarily SDG 3, but also SDG 1 (No Poverty) and SDG 10 (Reduced Inequalities).
-
Expiration of Enhanced Premium Tax Credits
The scheduled expiration of enhanced premium tax credits at the end of 2025 is a primary contributor to premium increases. This policy change directly undermines several SDG targets:
- SDG 3.8 (Universal Health Coverage): Insurers anticipate that the loss of subsidies will cause out-of-pocket premium payments to rise by an average of over 75%. This loss of financial protection is expected to force healthier individuals to drop their coverage, leading to a sicker, more expensive risk pool and further jeopardizing affordable access for those who remain. Insurers are adding an estimated 4% to premiums in anticipation of this effect.
- SDG 1 (No Poverty) & SDG 10 (Reduced Inequalities): The substantial increase in healthcare costs for individuals and families threatens to push vulnerable households into poverty and exacerbates existing inequalities by making essential health services unaffordable for lower-income populations.
-
Underlying Medical Cost Trend
The consistent rise in the cost and utilization of medical services and pharmaceuticals remains a fundamental driver. This trend, estimated at around 8% for 2026, presents an ongoing obstacle to sustainable healthcare financing.
- SDG 3.8 (Universal Health Coverage): Factors such as the high cost of new treatments like GLP-1 drugs and health care labor market pressures increase the baseline cost of care. This makes it progressively more difficult to provide quality, essential health-care services affordably, a core tenet of Target 3.8.
-
Economic Tariffs on Medical Goods
The imposition of tariffs on medical equipment, supplies, and pharmaceuticals is another factor contributing to higher costs. This has a clear negative impact on the affordability of essential health products.
- SDG 3.8 (Universal Health Coverage): Insurers that quantify this impact report that tariffs are driving premiums approximately 3% higher. This directly conflicts with the goal of ensuring access to affordable essential medicines and medical technologies for all.
-
Policy and Regulatory Uncertainty
Uncertainty surrounding the implementation of federal rules, such as the Marketplace Integrity and Affordability rule, and recent budget reconciliation legislation creates a volatile environment for insurers. While not a primary driver of rate changes thus far, such instability complicates long-term planning for sustainable health systems, which is essential for making consistent progress toward SDG 3.
Magnitude of Proposed Premium Changes for 2026
The proposed premium increases for 2026 are notably higher than in recent years, signaling a reversal of the market’s previous stability. This trend represents a significant setback for health affordability.
- The median proposed premium increase is 15% across the reviewed insurers.
- More than a quarter (27%) of insurers are proposing increases of 20% or more.
- In contrast, only 3% of insurers proposed increases of this magnitude for 2025.
- No insurers have filed for rate decreases for 2026, a departure from previous years where some premium reductions were observed.
These preliminary figures, which may be adjusted before finalization, indicate a substantial erosion of healthcare affordability. This trend directly threatens the nation’s ability to meet its commitments under the Sustainable Development Goals by moving away from, rather than toward, universal access to affordable health care and financial risk protection.
1. Which SDGs are addressed or connected to the issues highlighted in the article?
-
SDG 3: Good Health and Well-being
The article’s core subject is the affordability and accessibility of health insurance, which are fundamental components of a functioning health system. It discusses rising premiums, the cost of medical care, and prescription drugs, all of which directly relate to ensuring healthy lives and promoting well-being for all.
-
SDG 1: No Poverty
The article connects to SDG 1 by highlighting how rising healthcare costs and the expiration of financial assistance can lead to significant financial hardship. The expected “over 75%” increase in out-of-pocket premium payments for subsidized enrollees threatens the financial stability of vulnerable populations, pushing them closer to poverty.
-
SDG 10: Reduced Inequalities
The issues discussed relate to inequality in access to essential services. The article explains that the expiration of enhanced premium tax credits will disproportionately affect subsidized enrollees, likely causing healthier but less affluent individuals to drop their coverage. This creates a sicker, less equitable risk pool and widens the gap in healthcare access based on economic status.
2. What specific targets under those SDGs can be identified based on the article’s content?
-
SDG 3: Good Health and Well-being
-
Target 3.8: Achieve universal health coverage, including financial risk protection, access to quality essential health-care services and access to safe, effective, quality and affordable essential medicines and vaccines for all.
The article directly addresses this target by focusing on the challenges to financial risk protection and affordable healthcare. The discussion on rising premiums, the expiration of “enhanced premium tax credits,” and the increasing cost of “prescription drug costs” and “medical equipment” all point to the struggle to maintain affordable universal health coverage.
-
-
SDG 1: No Poverty
-
Target 1.3: Implement nationally appropriate social protection systems and measures for all, including floors, and by 2030 achieve substantial coverage of the poor and the vulnerable.
The “enhanced premium tax credits” described in the article serve as a social protection measure designed to make health coverage affordable for vulnerable populations. The article’s central concern is the negative impact of the expiration of this system, which will “cause premium payments for subsidized enrollees to increase by over 75%,” undermining this social protection floor.
-
-
SDG 10: Reduced Inequalities
-
Target 10.4: Adopt policies, especially fiscal, wage and social protection policies, and progressively achieve greater equality.
The article analyzes the impact of specific fiscal policies on equality. It examines how the potential expiration of tax credits (a social protection policy) and the imposition of “tariffs” (a fiscal policy) directly affect the affordability of health insurance, leading to greater inequality in access. The expectation that “healthier enrollees to drop their coverage” creating a “sicker risk pool” illustrates a regression from the goal of greater equality in health outcomes.
-
3. Are there any indicators mentioned or implied in the article that can be used to measure progress towards the identified targets?
-
Indicators for Target 3.8 (Universal Health Coverage)
- Median Premium Increase: The article states that “premiums are rising by a median of 15% in 2026,” which serves as a direct measure of the decreasing affordability of health coverage.
- Proportion of Insurers with High Rate Increases: The text notes that “more than a quarter (27%) of insurers are proposing premium increases of 20% or more for 2026,” compared to just 3% the previous year, indicating a widespread trend of rising costs for consumers.
- Medical Trend: The article cites that the “underlying cost of health care (medical trend) is similar to last year’s reported 8%,” which is an indicator of the rising cost of health services that insurers pass on to consumers.
-
Indicators for Target 1.3 (Social Protection Systems)
- Change in Out-of-Pocket Premium Payments: The article specifies that if tax credits expire, “premium payments for subsidized enrollees to increase by over 75% on average.” This is a clear indicator of the weakening of the social protection system.
- Impact of Subsidy Expiration on Premiums: Insurers are projected to “raise premiums by an additional 4%” in anticipation of the tax credits expiring, quantifying the direct impact of the policy change on affordability.
- Change in Health Insurance Enrollment: The article implies a negative change in enrollment, stating that “insurers expect a large share of enrollees to leave the market,” which can be used as an indicator of the failure of the system to provide substantial coverage for the vulnerable.
-
Indicators for Target 10.4 (Policies for Greater Equality)
- Impact of Tariffs on Premiums: The article quantifies the impact of a specific fiscal policy, noting that “the impact of tariffs on premiums is about 3%, on average,” which demonstrates how such policies can create financial barriers.
- Risk Pool Composition: The expectation that expiring subsidies will cause “healthier enrollees to drop their coverage and create a sicker risk pool” is an indicator of growing inequality, as the system becomes less viable and more expensive for those who remain, who are often those most in need of care.
4. Create a table with three columns titled ‘SDGs, Targets and Indicators” to present the findings from analyzing the article.
| SDGs | Targets | Indicators |
|---|---|---|
| SDG 3: Good Health and Well-being | 3.8: Achieve universal health coverage, including financial risk protection, access to quality essential health-care services and access to safe, effective, quality and affordable essential medicines and vaccines for all. |
|
| SDG 1: No Poverty | 1.3: Implement nationally appropriate social protection systems and measures for all, including floors, and by 2030 achieve substantial coverage of the poor and the vulnerable. |
|
| SDG 10: Reduced Inequalities | 10.4: Adopt policies, especially fiscal, wage and social protection policies, and progressively achieve greater equality. |
|
Source: healthsystemtracker.org