Report on Gut Microbiome Dynamics, Infectious Diseases, and Alignment with Sustainable Development Goals
This report synthesizes findings from a collection of scientific literature, focusing on the interplay between the gut microbiome, host immunity, and infectious diseases, particularly enteric fevers. The research presented holds significant implications for achieving several United Nations Sustainable Development Goals (SDGs), most notably SDG 3 (Good Health and Well-being) and SDG 6 (Clean Water and Sanitation).
The Gut Microbiome’s Role in Host Defense and Disease
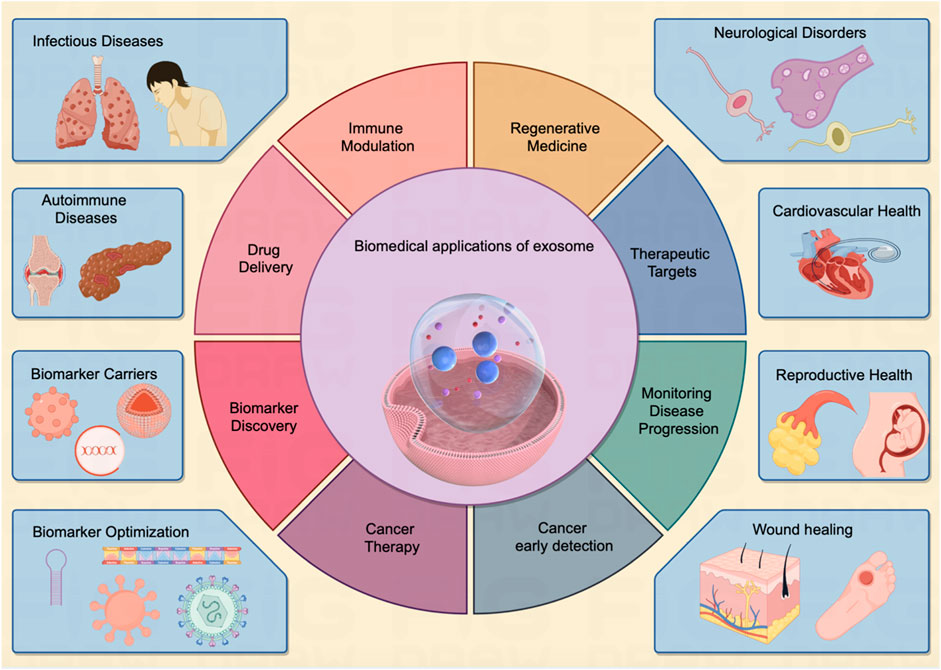
The human gut microbiome is a critical component of health, influencing immunity, inflammation, and resistance to pathogens. Understanding these dynamics is fundamental to advancing global health objectives outlined in SDG 3.
Microbiome-Mediated Immunity and Colonization Resistance
A healthy gut microbiota provides colonization resistance against enteric pathogens like Salmonella. This protective function is a key area of research with direct relevance to preventing communicable diseases.
- Commensal bacteria produce metabolites, such as butyrate, that promote regulatory T-cell generation and inhibit the expansion of pathogenic bacteria (Arpaia et al., 2013; Byndloss et al., 2017; Kullberg et al., 2024).
- The microbiota plays a well-established role in overall immunity and inflammation, highlighting its importance as a target for therapeutic intervention (Belkaid & Hand, 2014; Shreiner et al., 2015).
- Specific commensal-produced metabolites have been shown to directly mediate resistance to Salmonella infection, offering potential avenues for novel anti-infective strategies (Jacobson et al., 2018).
Dysbiosis and Association with Chronic and Infectious Diseases
Disruptions in the gut microbiome (dysbiosis) are linked to a variety of diseases, from inflammatory bowel disease (IBD) to colorectal cancer and increased susceptibility to infection. Addressing these links contributes to the SDG 3 target of reducing mortality from non-communicable diseases and ending epidemics.
- Studies have identified specific microbial signatures associated with colorectal cancer in diverse populations, such as in Morocco and Kenya (Allali et al., 2018; Obuya et al., 2022).
- Microorganisms linked to IBD-associated dysbiosis have been shown to differentially impact host physiology (Hoffmann et al., 2016).
- The composition of the gut microbiome has been correlated with clinical outcomes following infection with Salmonella Typhi, suggesting that the pre-infection state of the microbiome can determine disease severity (Zhang et al., 2018).
Enteric Fever: A Global Health Challenge Linked to SDG 3 and SDG 6
Typhoid and paratyphoid fevers remain a significant global burden, particularly in low- and middle-income countries. Research into their transmission, pathogenesis, and prevention is crucial for achieving SDG 3.3 (end the epidemics of communicable diseases) and SDG 6 (ensure availability and sustainable management of water and sanitation for all).
Global Burden and Environmental Risk Factors
The transmission of enteric fever is closely tied to environmental conditions, especially access to safe water and sanitation.
- Systematic analyses confirm the substantial global burden of typhoid and paratyphoid fevers, underscoring the need for integrated control strategies (Stanaway et al., 2019; Meiring et al., 2021).
- Risk factors identified in endemic areas like Jakarta, Indonesia, and Blantyre, Malawi, include contaminated food and water sources, directly linking disease incidence to the goals of SDG 6 (Vollaard et al., 2004; Gauld et al., 2020).
- Asymptomatic carriage and stool shedding of S. Typhi are critical for sustained transmission in endemic communities, complicating eradication efforts (Khanam et al., 2021; Qureshi et al., 2024).
Pathogenesis and Host-Pathogen Interactions
Understanding how Salmonella interacts with the host and its resident microbiota is key to developing effective vaccines and treatments.
- Salmonella exploits host inflammation to outcompete the native microbiota, often by using inflammation-derived compounds as respiratory electron acceptors (Stecher et al., 2007; Winter et al., 2010).
- Host immune responses, including the roles of interferon-γ and the IL-23 axis, are critical in controlling Salmonella infection (Bao et al., 2000; Godinez et al., 2011).
- Recent studies show how Salmonella can re-engineer the intestinal environment to overcome colonization resistance even in the presence of an intact microbiota (Rogers et al., 2024).
Antimicrobial Resistance (AMR) and Global Surveillance
The rise of AMR is a critical threat to global health security and a major impediment to achieving SDG 3. Genomic surveillance and understanding AMR transmission are paramount.
Tracking AMR Through Global Partnerships and Technology
International collaboration and advanced bioinformatics are essential tools in the fight against AMR, directly supporting SDG 17 (Partnerships for the Goals).
- Global resources like Pathogenwatch provide platforms for genomic prediction and surveillance of AMR in pathogens such as S. Typhi (Argimón et al., 2021).
- The Comprehensive Antibiotic Resistance Database (CARD) is an expanding resource that supports machine learning and resistome prediction, enhancing global capacity to monitor AMR (Alcock et al., 2023).
- Genomic epidemiological studies across countries like Bangladesh, Nepal, and Malawi have been instrumental in tracking the transmission of resistant Salmonella strains (Dyson et al., 2024).
Regional Trends in Antimicrobial Resistance
Surveillance studies from various regions highlight the local and global dimensions of the AMR crisis.
- A decade-long study in Dhaka, Bangladesh, documented the bacterial etiology and rising antimicrobial resistance in bloodstream infections (Ahmed et al., 2017).
- Long-term surveillance in Malawi (1998–2016) revealed significant trends in AMR in bloodstream infection isolates, providing critical data for local public health policy (Musicha et al., 2017).
- Understanding antimicrobial use patterns, such as among subsistence farmers in Malawi, is crucial for designing effective public awareness campaigns to curb AMR (MacPherson et al., 2022).
Comprehensive Reference List
- Ahmed D, Nahid MA, Sami AB, Halim F, Akter N, Tuhin Sadique Md, Sohel Rana Md, Elahi SB, Rahman MM. Bacterial etiology of bloodstream infections and antimicrobial resistance in Dhaka, Bangladesh, 2005–2014. Antimicrob Resist Infect Control. 2017;6(1):2.
- Alavi S, Mitchell JD, Cho JY, Liu R, Macbeth JC, Hsiao A. Interpersonal gut microbiome variation drives susceptibility and resistance to cholera infection. Cell. 2020;181(7):1533-1546.e13.
- Alcock BP, Huynh W, Chalil R, Smith KW, Raphenya AR, Wlodarski MA, Edalatmand A, et al. CARD 2023: expanded curation, support for machine learning, and resistome prediction at the comprehensive antibiotic resistance database. Nucleic Acids Res. 2023;51(D1):D690–9.
- Allali I, Boukhatem N, Bouguenouch L, Hanaa Hardi H, Abir Boudouaya M, Cadenas B, Ouldim K, Saaïd Amzazi M, Azcarate-Peril A, Ghazal H. Gut microbiome of moroccan colorectal cancer patients. Med Microbiol Immunol. 2018;207(3):211–25.
- Argimón S, Yeats CA, Goater RJ, Abudahab K, Taylor B, Underwood A, Sánchez-Busó L, et al. A global resource for genomic predictions of antimicrobial resistance and surveillance of Salmonella Typhi at Pathogenwatch. Nat Commun. 2021;12(1):2879.
- Arpaia N, Campbell C, Fan X, Dikiy S, van der Veeken J, Paul deRoos, Hui Liu, et al. Metabolites produced by commensal bacteria promote peripheral regulatory T-cell generation. Nature. 2013;504(7480):451–5.
- Bao S, Beagley KW, France MP, Shen J, Husband AJ. Interferon-γ plays a critical role in intestinal immunity against Salmonella Typhimurium Infection. Immunology. 2000;99(3):464–72.
- Belkaid Y, Hand T. Role of the microbiota in immunity and inflammation. Cell. 2014;157(1):121–41.
- Bilotta AJ, Cong Y. Gut microbiota metabolite regulation of host defenses at mucosal surfaces: implication in precision medicine. Precision Clinical Medicine. 2019;2(2):110–9.
- Blanco-Míguez A, Beghini F, Cumbo F, McIver LJ, Thompson KN, Zolfo M, Manghi P, et al. Extending and improving metagenomic taxonomic profiling with uncharacterized species using MetaPhlAn 4. Nat Biotechnol. 2023;41(11):1633–44.
- Blohmke CJ, Darton TC, Jones C, Suarez NM, Waddington CS, Angus B, Zhou L, et al. Interferon-driven alterations of the host’s amino acid metabolism in the pathogenesis of typhoid fever. J Exp Med. 2016;213(6):1061–77.
- Bohnhoff M, Drake BL, Phillip Miller C. Effect of Streptomycin on susceptibility of intestinal tract to experimental Salmonella infection. Proc Soc Exp Biol Med. 1954;86(1):132–7.
- Bourdeau-Julien I, Castonguay-Paradis S, Rochefort G, Perron J, Lamarche B, Flamand N, Di Marzo V, Veilleux A, Raymond F. The diet rapidly and differentially affects the gut microbiota and host lipid mediators in a healthy population. Microbiome. 2023;11(1):26.
- Bunker, Jeffrey J., Christoph Drees, Andrea R. Watson, Catherine H. Plunkett, Cathryn R. Nagler, Olaf Schneewind, A. Murat Eren, and Albert Bendelac. 2019. B cell superantigens in the human intestinal microbiota. Sci Translat Med. 11 (507): eaau9356.
- Byndloss MX, Olsan EE, Rivera-Chávez F, Tiffany CR, Cevallos SA, Lokken KL, Torres TP, et al. Microbiota-activated PPAR-γ signaling inhibits dysbiotic enterobacteriaceae expansion. Science. 2017;357(6351):570–5.
- Chuttani HK, Jain K, Misra RC. Small bowel in typhoid fever Gut. 1971;12(9):709–12.
- Constantinides, Bede, Martin Hunt, and Derrick W Crook. 2023. Hostile: accurate decontamination of microbial host sequences. Bioinformatics. 39 (12): btad728.
- Darton TC, Meiring JE, Susan Tonks Md, Khan A, Khanam F, Shakya M, Thindwa D, et al. The STRATAA study protocol: a programme to assess the burden of enteric fever in Bangladesh, Malawi and Nepal using prospective population census, passive surveillance, serological studies and healthcare utilisation surveys’. BMJ Open. 2017;7(6): e016283.
- Durack J, Lynch SV. The gut microbiome: relationships with disease and opportunities for therapy. J Exp Med. 2019;216(1):20–40.
- Dyson, Zoe A., Philip M. Ashton, Farhana Khanam, Angeziwa Chunga Chirambo, Mila Shakya, James E. Meiring, Susan Tonks, et al. 2024. Pathogen diversity and antimicrobial resistance transmission of Salmonella Enterica Serovars Typhi and Paratyphi A in Bangladesh, Nepal, and Malawi: a genomic epidemiological study. The Lancet Microbe. 0 (0).
- Faber F, Thiennimitr P, Spiga L, Byndloss MX, Litvak Y, Lawhon S, Andrews-Polymenis HL, Winter SE, Bäumler AJ. Respiration of microbiota-derived 1,2-propanediol drives Salmonella expansion during colitis. PLoS Pathog. 2017;13(1): e1006129.
- Gauld JS, Olgemoeller F, Nkhata R, Li C, Chirambo A, Morse T, Gordon MA, et al. Domestic river water use and risk of typhoid fever: results from a case-control study in Blantyre. Malawi Clinical Infectious Diseases. 2020;70(7):1278–84.
- Gibani MM, Jin C, Shrestha S, Moore M, Norman L, Voysey M, Jones E, et al. Homologous and heterologous re-challenge with Salmonella Typhi and Salmonella Paratyphi A in a randomised controlled human infection model. PLoS Negl Trop Dis. 2020;14(10): e0008783.
- Godinez I, Marijke Keestra A, Spees A, Bäumler AJ. The IL-23 axis in Salmonella Gastroenteritis. Cell Microbiol. 2011;13(11):1639–47.
- Gül E, Younes AA, Huuskonen J, Diawara C, Nguyen BD, Maurer L, Bakkeren E, Hardt W-D. Differences in carbon metabolic capacity fuel co-existence and plasmid transfer between Salmonella strains in the mouse gut. Cell Host Microbe. 2023;31(7):1140-1153.e3.
- Gupta VK, Paul S, Dutta C. Geography, ethnicity or subsistence-specific variations in human microbiome composition and diversity. Front Microbiol. 2017;8(June):1162.
- Haak, Bastiaan W, Hanna K de Jong, Sarantos Kostidis, Martin Giera, Rapeephan R Maude, Rasheda Samad, Lalith Wijedoru, et al. 2020. Altered patterns of compositional and functional disruption of the gut microbiota in typhoid fever and nontyphoidal febrile illness. Open Forum Infectious Diseases. 7 (7).
- Hoffmann TW, Pham H-P, Bridonneau C, Aubry C, Lamas B, Martin-Gallausiaux C, Moroldo M, et al. Microorganisms linked to inflammatory bowel disease-associated dysbiosis differentially impact host physiology in gnotobiotic mice. ISME J. 2016;10(2):460–77.
- Hollister EB, Riehle K, Luna RA, Weidler EM, Rubio-Gonzales M, Mistretta T-A, Raza S, et al. Structure and function of the healthy pre-adolescent pediatric gut microbiome. Microbiome. 2015;3(August):36.
- Huus, Kelsey E., and Ruth E. Ley. 2021. Blowing hot and cold: body temperature and the microbiome. mSystems 6 (5).
- Jacobson A, Lam L, Rajendram M, Tamburini F, Honeycutt J, Pham T, Van Treuren W, et al. A gut commensal-produced metabolite mediates colonization resistance to Salmonella infection. Cell Host Microbe. 2018;24(2):296-307.e7.
- Khanam F, Darton TC, Meiring JE, Sarker PK, Biswas PK, Bhuiyan MAI, Rajib NH, et al. Salmonella Typhi stool shedding by patients with enteric fever and asymptomatic chronic carriers in an endemic urban setting. J Infect Dis. 2021;224(12 Suppl 2):S759–63.
- Kullberg RFJ, Wikki I, Haak BW, Kauko A, Galenkamp H, Peters-Sengers H, Butler JM, et al. Association between butyrate-producing gut bacteria and the risk of infectious disease hospitalisation: results from two observational, population-based microbiome studies. The Lancet Microbe. 2024;5(9): 100864.
- Larsen JM. The immune response to prevotella bacteria in chronic inflammatory disease. Immunology. 2017;151(4):363–74.
- Lee J-Y, Arai H, Nakamura Y, Fukiya S, Wada M, Yokota A. Contribution of the 7β-hydroxysteroid dehydrogenase from Ruminococcus Gnavus N53 to ursodeoxycholic acid formation in the human colon. J Lipid Res. 2013;54(11):3062–9.
- Leshem A, Liwinski T, Elinav E. Immune-microbiota interplay and colonization resistance in infection. Mol Cell. 2020;78(4):597–613.
- Libertucci J, Young VB. The role of the microbiota in infectious diseases. Nat Microbiol. 2019;4(1):35–45.
- Lopez, Christopher A., Brittany M. Miller, Fabian Rivera-Chávez, Eric M. Velazquez, Mariana X. Byndloss, Alfredo Chávez-Arroyo, Kristen L. Lokken, Renée M. Tsolis, Sebastian E. Winter, and Andreas J. Bäumler. 2016. Virulence factors enhance Citrobacter Rodentium expansion through aerobic respiration. Science (New York, N.Y.) 353 (6305): 1249–53.
- MacPherson EE, Reynolds J, Sanudi E, Nkaombe A, Mankhomwa J, Dixon J, Chandler CIR. Understanding antimicrobial use in subsistence farmers in Chikwawa District Malawi, implications for public awareness campaigns. PLOS Global Public Health. 2022;2(6): e0000314.
- Mallick H, Rahnavard A, McIver LJ, Ma S, Zhang Y, Nguyen LH, Tickle TL, et al. Multivariable association discovery in population-scale meta-omics studies. PLoS Comput Biol. 2021;17(11): e1009442.
- McGrath, Conor J., Edgaras Laveckis, Andrew Bell, Emmanuelle Crost, Nathalie Juge, and Stephanie Schüller. 2022. Development of a novel human intestinal model to elucidate the effect of anaerobic commensals on Escherichia coli infection. Disease Models & Mechanisms. 15 (4): dmm049365.
- Meiring JE, Khanam F, Basnyat B, Charles RC, Crump JA, Debellut F, Holt KE, et al. Typhoid fever. Nat Rev Dis Primers. 2023;9(1):1–18.
- Meiring JE, Shakya M, Khanam F, Voysey M, Phillips MT, Tonks S, Thindwa D, et al. Burden of enteric fever at three urban sites in Africa and Asia: a multicentre population-based study. Lancet Glob Health. 2021;9(12):e1688–96.
- Musicha P, Cornick JE, Bar-Zeev N, French N, Masesa C, Denis B, Kennedy N, et al. Trends in antimicrobial resistance in bloodstream infection isolates at a large urban hospital in Malawi (1998–2016): a surveillance study. Lancet Infect Dis. 2017;17(10):1042–52.
- Obuya, Sarah, Amr Elkholy, Nagavardhini Avuthu, Michael Behring, Prachi Bajpai, Sumit Agarwal, Hyung-Gyoon Kim, et al. 2022. A signature of Prevotella Copri and Faecalibacterium Prausnitzii depletion, and a link with bacterial glutamate degradation in the Kenyan colorectal cancer patients. J Gastro Oncol. 13 (5): 2282–92.
- Pascal Andreu, Victória, Hannah E. Augustijn, Koen van den Berg, Justin J. J. van der Hooft, Michael A. Fischbach, and Marnix H. Medema. 2021. BiG-MAP: an automated pipeline to profile metabolic gene cluster abundance and expression in microbiomes. mSystems. 6 (5): e00937–21.
- Andreu P, Victòria HE, Augustijn LC, Zhernakova A, Jingyuan Fu, Fischbach MA, Dodd D, Medema MH. gutSMASH predicts specialized primary metabolic pathways from the human gut microbiota. Nat Biotechnol. 2023;41(10):1416–23.
- Patel PD, Patel P, Liang Y, Meiring JE, Misiri T, Felistas Mwakiseghile J, Tracy K, et al. Safety and efficacy of a typhoid conjugate vaccine in Malawian Children. N Engl J Med. 2021;385(12):1104–15.
- Proietti E, Rossini S, Grohmann U, Mondanelli G. Polyamines and Kynurenines at the intersection of immune modulation. Trends Immunol. 2020;41(11):1037–50.
- Qureshi S, Maria N, Chawla T, Iqbal J, Kazi AM, Adnan M, Hotwani A, et al. The frequency and associated factors of typhoid carriage in patients undergoing cholecystectomy for gallbladder disease in Pakistan: a cross-sectional study. PLoS Negl Trop Dis. 2024;18(6): e0011775.
- Raffatellu M, Santos RL, Verhoeven DE, George MD, Paul Wilson R, Winter SE, Godinez I, et al. Simian immunodeficiency virus–induced mucosal interleukin-17 deficiency promotes Salmonella dissemination from the gut. Nat Med. 2008;14(4):421–8.
- Rao JN, Xiao L, Wang J-Y. Polyamines in gut epithelial renewal and barrier function. Physiology. 2020;35(5):328–37.
- Robbins JD, Robbins JB. Reexamination of the protective role of the capsular Polysaccharide (Vi antigen) of Salmonella Typhi. J Infect Dis. 1984;150(3):436–49.
- Rogers AWL, Radlinski LC, Nguyen H, Tiffany CR, Carvalho TP, Masson HLP, Goodson ML, et al. Salmonella re-engineers the intestinal environment to break colonization resistance in the presence of a compositionally intact microbiota. Cell Host Microbe. 2024;32(10):1774-1786.e9.
- Rogers AWL, Tsolis RM, Bäumler AJ. Salmonella versus the microbiome. Microbiol Mol Biol Rev. 2021;85(1):e00027-e119.
- Shreiner AB, Kao JY, Young VB. The gut microbiome in health and in disease. Curr Opin Gastroenterol. 2015;31(1):69–75.
- Sohn J, Li Lu, Zhang L, Genco RJ, Falkner KL, Tettelin H, Rowsam AM, et al. Periodontal disease is associated with increased gut colonization of pathogenic haemophilusparainfluenzae in patients with Crohn’s disease. Cell Rep. 2023;42(2): 112120.
- Song, Se Jin, Christian Lauber, Elizabeth K Costello, Catherine A Lozupone, Gregory Humphrey, Donna Berg-Lyons, J Gregory Caporaso, et al. 2013. Cohabiting family members share microbiota with one another and with their dogs. eLife. 2 (April):e00458.
- Stanaway JD, Reiner RC, Blacker BF, Goldberg EM, Khalil IA, Troeger CE, Andrews JR, et al. The global burden of typhoid and paratyphoid fevers: a systematic analysis for the global burden of disease study 2017. Lancet Infect Dis. 2019;19(4):369–81.
- Stecher B, Robbiani R, Walker AW, Westendorf AM, Barthel M, Kremer M, Chaffron S, et al. Salmonella Enterica Serovar typhimurium exploits inflammation to compete with the intestinal microbiota. PLoS Biol. 2007;5(10): e244.
- Steele AD, Hay DC, Burgess ZD, Carey ME, Zaidi AKM. Challenges and opportunities for typhoid fever control: a call for coordinated action. Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America. 2016;62(Suppl 1):S4-8.
- Valles-Colomer M, Blanco-Míguez A, Manghi P, Asnicar F, Dubois L, Golzato D, Armanini F, et al. The person-to-person transmission landscape of the gut and oral microbiomes. Nature. 2023;614(7946):125–35.
- Vollaard AM, Ali S, van Asten HAGH, Widjaja S, Visser LG, Surjadi C, van Dissel JT. Risk factors for typhoid and paratyphoid fever in Jakarta. Indonesia’ JAMA. 2004;291(21):2607–15.
- Waddington CS, Darton TC, Jones C, Haworth K, Peters A, John T, Thompson BAV, et al. An outpatient, ambulant-design, controlled human infection model using escalating doses of Salmonella Typhi challenge delivered in sodium bicarbonate solution. Clin Infect Dis. 2014;58(9):1230–40.
- Winter SE, Thiennimitr P, Winter MG, Butler BP, Huseby DL, Crawford RW, Russell JM, et al. Gut inflammation provides a respiratory electron acceptor for Salmonella. Nature. 2010;467(7314):426–9.
- Yang X, Stein KR, Hang HC. Anti-infective bile acids bind and inactivate a Salmonella virulence regulator. Nat Chem Biol. 2023;19(1):91–100.
- Yatsunenko T, Rey FE, Manary MJ, Trehan I, Dominguez-Bello MG, Contreras M, Magris M, et al. Human gut microbiome viewed across age and geography. Nature. 2012;486(7402):222–7.
- Zhang, Yan, Arthur Brady, Cheron Jones, Yang Song, Thomas C. Darton, Claire Jones, Christoph J. Blohmke, et al. 2018. Compositional and functional differences in the human gut microbiome correlate with clinical outcome following infection with wild-type Salmonella Enterica Serovar Typhi. mBio. 9 (3): e00686–18.
- Zhu W, Winter MG, Byndloss MX, Spiga L, Duerkop BA, Hughes ER, Büttner L, et al. Precision editing of the gut microbiota ameliorates colitis. Nature. 2018;553(7687):208–11.
SDGs, Targets, and Indicators Analysis
Which SDGs are addressed or connected to the issues highlighted in the article?
The provided list of references primarily focuses on research related to infectious diseases, gut health, and public health surveillance, which directly connects to several Sustainable Development Goals (SDGs). The main SDGs addressed are:
-
SDG 3: Good Health and Well-being
This is the most prominent SDG, as the majority of the references investigate health-related issues. The articles cover the etiology of bloodstream infections (Ref 1), antimicrobial resistance (Ref 1, 3, 5, 44), the burden and control of specific infectious diseases like typhoid and paratyphoid fever (Ref 18, 20, 42, 43, 59, 61), the role of the gut microbiome in health and disease (Ref 8, 19, 56), and the development and efficacy of vaccines (Ref 48).
-
SDG 6: Clean Water and Sanitation
This goal is addressed through its direct link to water-borne diseases. Enteric fevers like typhoid are often transmitted through contaminated water and food. Reference 22 explicitly investigates the “Domestic river water use and risk of typhoid fever,” directly linking water source quality to health outcomes. Other studies on typhoid in endemic areas (Ref 18, 63) implicitly highlight the challenges related to water and sanitation infrastructure.
-
SDG 17: Partnerships for the Goals
The collaborative nature of the research cited is evident, pointing to the importance of partnerships. Many studies involve international collaborations across multiple institutions and countries (e.g., the STRATAA study in Bangladesh, Malawi, and Nepal, Ref 18, 20, 43). Furthermore, the development of global resources for surveillance and data sharing, such as the Comprehensive Antibiotic Resistance Database (CARD) (Ref 3) and Pathogenwatch (Ref 5), exemplifies global partnerships to tackle health challenges.
What specific targets under those SDGs can be identified based on the article’s content?
Based on the topics of the references, several specific SDG targets can be identified:
SDG 3: Good Health and Well-being
-
Target 3.3: By 2030, end the epidemics of AIDS, tuberculosis, malaria and neglected tropical diseases and combat hepatitis, water-borne diseases and other communicable diseases.
The extensive research on typhoid and paratyphoid fevers (Ref 20, 42, 59), cholera (Ref 2), and Salmonella infections (Ref 7, 55, 60) directly contributes to understanding and combating these major water-borne and communicable diseases.
-
Target 3.b: Support the research and development of vaccines and medicines for the communicable and non-communicable diseases that primarily affect developing countries…
The article list includes research on the “Safety and efficacy of a typhoid conjugate vaccine in Malawian Children” (Ref 48) and studies on human infection models (Ref 23, 64) used to test vaccines and treatments, directly aligning with this target.
-
Target 3.d: Strengthen the capacity of all countries, in particular developing countries, for early warning, risk reduction and management of national and global health risks.
This target is supported by studies on antimicrobial resistance surveillance (Ref 1, 44), the development of global genomic surveillance platforms like Pathogenwatch (Ref 5), and research assessing the burden of enteric fever to inform public health policy (Ref 18, 43).
SDG 6: Clean Water and Sanitation
-
Target 6.1: By 2030, achieve universal and equitable access to safe and affordable drinking water for all.
The study linking “domestic river water use and risk of typhoid fever” in Malawi (Ref 22) provides critical evidence of the health consequences of lacking access to safe water, reinforcing the importance of this target and providing data to monitor risks associated with unsafe sources.
SDG 17: Partnerships for the Goals
-
Target 17.6: Enhance North-South, South-South and triangular regional and international cooperation on and access to science, technology and innovation…
The multi-country studies assessing the burden of enteric fever in Bangladesh, Malawi, and Nepal (Ref 18, 43) and the genomic epidemiology study across these nations (Ref 20) are clear examples of international scientific cooperation to address shared health problems.
Are there any indicators mentioned or implied in the article that can be used to measure progress towards the identified targets?
Yes, the references mention or imply several indicators that can be used to measure progress:
- Incidence and Burden of Disease: Several studies focus on assessing the “burden of enteric fever” (Ref 18, 43) and the “global burden of typhoid and paratyphoid fevers” (Ref 59). The incidence rates and mortality data from such studies are direct indicators for tracking progress on Target 3.3.
- Trends in Antimicrobial Resistance (AMR): Research on “antimicrobial resistance in bloodstream infections” in Dhaka (Ref 1) and Malawi (Ref 44) provides data on the prevalence of resistant pathogens. The proportion of infections that are resistant to standard antibiotics is a key indicator for Target 3.d, measuring a critical global health risk.
- Vaccine Efficacy and Coverage: The study on the “safety and efficacy of a typhoid conjugate vaccine” (Ref 48) provides a direct indicator of the effectiveness of a public health intervention. Vaccine efficacy rates from clinical trials are crucial for implementing vaccination programs aimed at achieving Target 3.b.
- Identification of Disease Risk Factors: Studies that identify and quantify risk factors, such as the link between “domestic river water use and risk of typhoid fever” (Ref 22) or risk factors in Jakarta (Ref 63), provide indicators of environmental and behavioral risks. These help measure progress towards Target 6.1 by highlighting populations that lack access to safe water.
- Development of Global Health Resources: The creation and use of global databases like the “Comprehensive Antibiotic Resistance Database (CARD)” (Ref 3) and surveillance platforms like “Pathogenwatch” (Ref 5) serve as indicators of enhanced global cooperation and capacity for health risk management (Targets 17.6 and 3.d).
Summary Table of SDGs, Targets, and Indicators
| SDGs | Targets | Indicators (with reference examples) |
|---|---|---|
| SDG 3: Good Health and Well-being | 3.3: End epidemics of communicable diseases. | Incidence and burden of enteric fevers (Ref: 43, 59). |
| SDG 3: Good Health and Well-being | 3.d: Strengthen early warning and risk management. | Trends in antimicrobial resistance in bloodstream infections (Ref: 1, 44). |
| SDG 3: Good Health and Well-being | 3.b: Support R&D of vaccines and medicines. | Efficacy rate of new vaccines (e.g., typhoid conjugate vaccine) (Ref: 48). |
| SDG 6: Clean Water and Sanitation | 6.1: Achieve access to safe drinking water. | Documented risk of disease from unsafe water sources (Ref: 22). |
| SDG 17: Partnerships for the Goals | 17.6: Enhance international cooperation on science and technology. | Execution of multi-country research programs and development of global data platforms (Ref: 18, 20, 5). |
Source: microbiomejournal.biomedcentral.com