Report on Diabetes Classification and its Implications for Sustainable Development Goals
The global health landscape is significantly impacted by the rising prevalence of diabetes, a non-communicable disease that poses a substantial challenge to achieving Sustainable Development Goal 3 (Good Health and Well-being). While Type 1 and Type 2 diabetes are widely recognized, recent developments have brought attention to Malnutrition-Related Diabetes Mellitus (MRDM), a distinct form of the disease with profound connections to several SDGs.
Understanding Diabetes Types in the Context of Global Health
H3: Established Forms of Diabetes
A clear understanding of different diabetes classifications is essential for effective public health strategies. The primary recognized types include:
- Type 1 Diabetes: An autoimmune condition where the pancreas produces insufficient insulin. It accounts for 5-10% of cases and is not reversible.
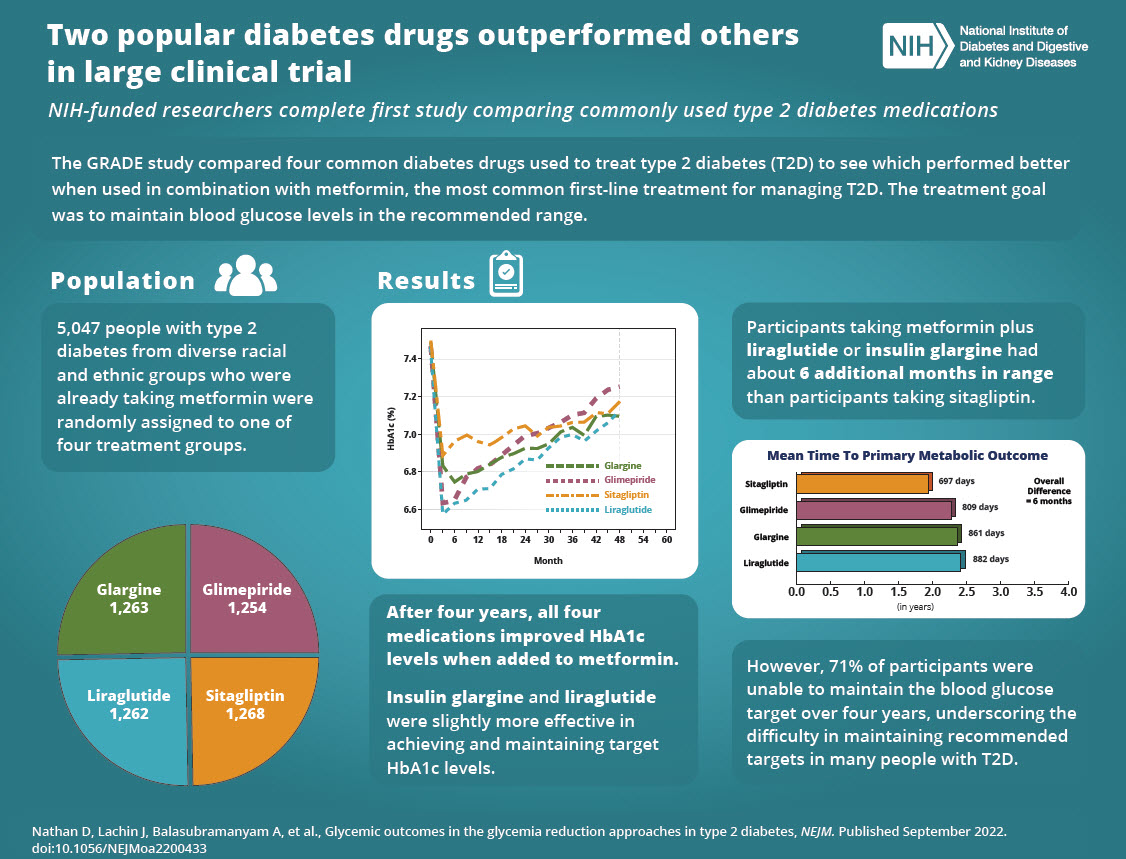
- Type 2 Diabetes: Characterized by insulin resistance, this type constitutes 90-95% of cases and is strongly linked to lifestyle factors, obesity, and age. Addressing Type 2 diabetes is a key component of promoting healthy lifestyles under SDG 3.
- Other Forms: Gestational diabetes (occurring during pregnancy) and Type 3c (resulting from pancreatic diseases) are also established classifications.
H3: The Emergence of Malnutrition-Related Diabetes Mellitus (MRDM)
Researchers and international bodies are now advocating for the formal classification of MRDM, also referred to as Type 5 diabetes. This condition is fundamentally linked to socio-economic factors and directly impacts the achievement of multiple SDGs.
- Cause: MRDM develops in individuals with a low Body Mass Index (BMI) who have experienced chronic undernutrition, particularly during developmental stages.
- Mechanism: Unlike Type 2 diabetes, MRDM is not primarily caused by insulin resistance. Instead, chronic malnutrition leads to the pancreas underproducing insulin.
- Symptoms: Common indicators include significant weight loss, fatigue, frequent urination, and increased susceptibility to infections.
MRDM: A Critical Intersection of Health, Poverty, and Hunger
The recognition of MRDM is not merely a clinical distinction; it is a crucial step in addressing systemic global challenges reflected in the Sustainable Development Goals.
H3: Link to SDG 2 (Zero Hunger) and SDG 1 (No Poverty)
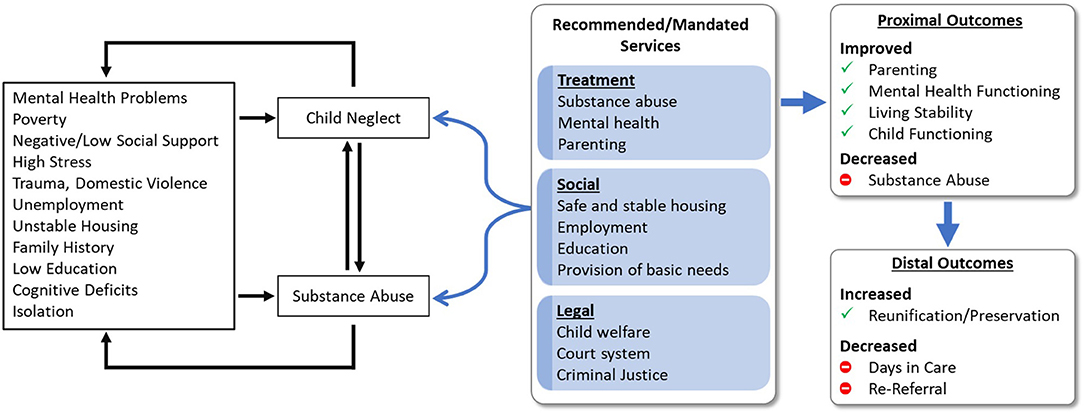
MRDM is a direct physiological manifestation of food insecurity and poverty. Its prevalence highlights a failure to achieve basic nutritional standards, a core target of SDG 2. As malnutrition is often a consequence of poverty, tackling MRDM is intrinsically linked to the objectives of SDG 1.
H3: Implications for SDG 3 (Good Health and Well-being) and SDG 10 (Reduced Inequalities)
Properly classifying MRDM is vital for ensuring effective health outcomes. Misdiagnosing it as Type 1 or Type 2 can lead to inappropriate and potentially harmful treatment protocols.
- Health Equity: Recognizing MRDM addresses significant health disparities, ensuring that vulnerable, malnourished populations receive accurate diagnoses and tailored care, thereby advancing SDG 10.
- Targeted Treatment: The management of MRDM focuses on nutritional rehabilitation and carefully controlled insulin therapy to avoid hypoglycemia, a different approach than standard Type 1 or Type 2 treatments. This specialized care is essential for fulfilling the promise of universal health coverage under SDG 3.
Global Recognition and Path Forward
H3: International Classification Efforts
The International Diabetes Federation (IDF) has formally acknowledged MRDM as Type 5 diabetes, launching a working group to establish clear diagnostic and treatment criteria. This move underscores the importance of global cooperation in addressing health challenges.
H3: The Role of SDG 17 (Partnerships for the Goals)
Despite the IDF’s recognition, formal classification by the World Health Organization (WHO) and the American Diabetes Association (ADA) is still pending. Achieving a global consensus requires robust international collaboration among medical bodies, governments, and non-governmental organizations, embodying the spirit of SDG 17. A unified approach is necessary to ensure that MRDM is integrated into global health policies, thereby addressing the interconnected issues of health, hunger, and inequality.
Analysis of Sustainable Development Goals (SDGs) in the Article
1. Which SDGs are addressed or connected to the issues highlighted in the article?
-
SDG 3: Good Health and Well-being
- The article’s primary focus is on diabetes, a major non-communicable disease (NCD). It discusses the prevalence of diabetes in the U.S. (“Nearly 39 million American adults are currently living with diabetes”), describes different types (Type 1, 2, and 5), and details their causes, symptoms, and treatments. This directly relates to ensuring healthy lives and promoting well-being for all at all ages.
-
SDG 2: Zero Hunger
- The article introduces “type 5 diabetes, or malnutrition-related diabetes mellitus (MRDM).” It explicitly states that this condition is the result of “chronic undernutrition” and develops in people “who were chronically malnourished during development and adulthood.” This connects the health issue directly to the goal of ending hunger, achieving food security, and improving nutrition.
-
SDG 10: Reduced Inequalities
- The article mentions that MRDM is a result of “chronic undernutrition and health disparities.” The term “health disparities” implies that this form of diabetes disproportionately affects vulnerable or disadvantaged populations who lack access to adequate nutrition. This highlights the link between health outcomes and inequality.
2. What specific targets under those SDGs can be identified based on the article’s content?
-
Target 3.4: Reduce premature mortality from non-communicable diseases
- By 2030, reduce by one third premature mortality from non-communicable diseases through prevention and treatment and promote mental health and well-being. The article contributes to this target by raising awareness about different forms of diabetes, discussing lifestyle factors linked to Type 2 diabetes (“obesity and unhealthy lifestyle factors”), and outlining diagnostic and treatment approaches (“Treatment focuses on nutritional rehabilitation… Oral medications and a high-protein diet are also part of the management plan”).
-
Target 2.2: End all forms of malnutrition
- By 2030, end all forms of malnutrition, including achieving, by 2025, the internationally agreed targets on stunting and wasting in children under 5 years of age, and address the nutritional needs of adolescent girls, pregnant and lactating women and older persons. The article directly addresses this target by identifying “chronic undernutrition” as the root cause of Type 5 diabetes. The diagnostic criteria mentioned, such as a “history of malnutrition” and “low BMI,” are central to the goals of ending malnutrition.
3. Are there any indicators mentioned or implied in the article that can be used to measure progress towards the identified targets?
-
Prevalence of diabetes
- The article begins with a clear statistic: “Nearly 39 million American adults are currently living with diabetes.” This figure serves as a direct indicator for monitoring the burden of non-communicable diseases, relevant to Target 3.4. Tracking this number over time would measure progress in managing and preventing diabetes.
-
Prevalence of malnutrition and low Body Mass Index (BMI)
- The article states that a diagnosis of type 5 diabetes involves “assessing a history of malnutrition, low BMI and age under 30 at diagnosis.” The prevalence of low BMI and documented cases of chronic malnutrition within a population are measurable indicators that directly relate to Target 2.2. A reduction in these indicators would signify progress in ending malnutrition.
-
Incidence of disease linked to health disparities (implied)
- The article links Type 5 diabetes to “health disparities.” While not providing a specific number, this implies an indicator: the rate of MRDM among different socioeconomic or geographic groups. Measuring and tracking the incidence of this disease in vulnerable populations versus the general population would be an effective way to monitor progress in reducing health inequalities (related to SDG 10).
Summary Table of SDGs, Targets, and Indicators
| SDGs | Targets | Indicators |
|---|---|---|
| SDG 3: Good Health and Well-being | 3.4: By 2030, reduce by one third premature mortality from non-communicable diseases through prevention and treatment. | Prevalence of diabetes (e.g., “Nearly 39 million American adults are currently living with diabetes”). |
| SDG 2: Zero Hunger | 2.2: By 2030, end all forms of malnutrition. | Prevalence of malnutrition and low Body Mass Index (BMI) (e.g., Diagnosis involves assessing a “history of malnutrition, low BMI”). |
| SDG 10: Reduced Inequalities | 10.2 (Implied): By 2030, empower and promote the social, economic and political inclusion of all. | Incidence of disease linked to health disparities (Implied by the mention of “health disparities” as a cause of MRDM). |
Source: foxnews.com