Report on Advanced Sterilization Assurance for Medical Devices in Alignment with Sustainable Development Goals
SDG 3: Good Health and Well-being
Achieving reliable sterility assurance is fundamental to global public health, directly supporting the objectives of SDG 3. The validation of sterilization processes for medical and IVD products ensures patient safety by preventing infections.
- Enhanced Safety Benchmarks: The adoption of an 8-spore log reduction (SLR) as a benchmark for complete microbial kill provides a higher margin of safety than the common 6-log assumption, significantly reducing the risk of healthcare-associated infections.
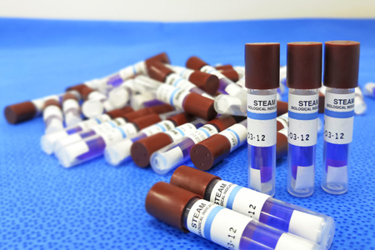
- Reliable Verification: The correct selection and use of biological indicators (BIs), such as self-contained biological indicators (SCBIs), and Process Challenge Devices (PCDs) are critical for verifying the efficacy of every sterilization cycle.
- Consistent Process Control: Best practices in handling and load configuration ensure that sterility is consistently achieved, safeguarding the well-being of patients who rely on these medical devices.
SDG 9: Industry, Innovation, and Infrastructure
The methodologies for Ethylene Oxide (EO) sterilization validation represent significant innovation in industrial processes, contributing to a resilient and technologically advanced healthcare manufacturing infrastructure as outlined in SDG 9.
- Advanced Validation Methods: The application of the overkill method and precise D-value calculations are sophisticated validation strategies that enhance the reliability and efficiency of industrial sterilization.
- Compliance with Global Standards: Adherence to international standards, specifically ISO 11135, promotes quality, innovation, and regulatory confidence, ensuring that sterilization infrastructure meets globally recognized benchmarks for safety and effectiveness.
- Strategic Process Design: The selection of internal versus external PCDs must be aligned with the most challenging sterilization scenarios, demonstrating an innovative and risk-based approach to process validation and industrial quality control.
SDG 12: Responsible Consumption and Production
Effective sterilization strategies contribute to sustainable production patterns within the medical device industry, aligning with the principles of SDG 12.
- Waste Reduction: A robust and validated sterilization process minimizes the risk of batch failures. This prevents the unnecessary disposal of entire loads of medical devices, thereby reducing product waste and conserving the raw materials and energy used in their production.
- Resource Efficiency: By ensuring a complete and reliable kill with the first cycle, validated procedures prevent the need for costly and resource-intensive re-sterilization, promoting efficient use of chemicals and energy.
- Ensuring Product Viability: Proper selection of PCD configurations ensures that products are not over-exposed or under-exposed to the sterilant, maintaining product integrity and ensuring that resources invested in manufacturing are not wasted due to process deviations.
Analysis of Sustainable Development Goals (SDGs) in the Article
1. Relevant SDGs
-
SDG 3: Good Health and Well-being
- The article’s entire focus is on the sterilization of medical devices to achieve “reliable sterility assurance.” This process is fundamental to preventing infections during medical procedures, ensuring patient safety, and upholding the quality of healthcare services, which directly aligns with the goal of ensuring healthy lives and promoting well-being.
-
SDG 9: Industry, Innovation, and Infrastructure
- The text discusses highly technical industrial processes, including “EO sterilization,” “validation strategies,” and compliance with international standards like “ISO 11135.” This relates to building quality and reliable infrastructure, promoting sustainable industrialization, and fostering innovation within the medical technology sector.
2. Specific Targets
-
Target 3.d: Strengthen the capacity of all countries, in particular developing countries, for early warning, risk reduction and management of national and global health risks.
- The article directly addresses this target by detailing advanced methods for sterilizing medical equipment. Proper sterilization is a critical component of managing the health risk of hospital-acquired infections. The pursuit of an “8-log spore reduction” and “regulatory confidence” demonstrates a strategy to strengthen risk reduction in healthcare settings.
-
Target 9.1: Develop quality, reliable, sustainable and resilient infrastructure, including regional and transborder infrastructure, to support economic development and human well-being, with a focus on affordable and equitable access for all.
- The emphasis on “ISO 11135 compliance requirements” and robust “validation strategies” contributes directly to the development of quality and reliable industrial infrastructure. These standards and processes ensure that the medical devices produced and used are safe, supporting human well-being.
-
Target 9.5: Enhance scientific research, upgrade the technological capabilities of industrial sectors in all countries, in particular developing countries, including, by 2030, encouraging innovation and substantially increasing the number of research and development workers per 1 million people and public and private research and development spending.
- The article’s discussion of “D-value calculations,” the selection of “Process Challenge Device (PCD) configuration,” and the use of different “BI formats” like “SCBIs” are all examples of upgrading technological capabilities and applying scientific research within the sterilization industry to improve outcomes.
3. Mentioned or Implied Indicators
-
Spore Log Reduction (SLR) Level
- The article explicitly proposes an “8-log spore reduction (SLR)” as a “more accurate benchmark for complete kill.” This is a specific, quantifiable performance indicator used to measure the effectiveness of the sterilization process, thereby measuring progress towards ensuring health safety (Target 3.d).
-
Compliance with International Standards
- The reference to “ISO 11135 compliance requirements” serves as a clear indicator. Adherence to this standard measures the quality of the industrial process (Target 9.1) and the capacity to manage health risks associated with medical devices (Target 3.d).
-
Application of Specific Scientific Methods and Technologies
- The mention of “D-value calculations” and the use of advanced tools like “Process Challenge Devices (PCDs)” and “self-contained biological indicators (SCBIs)” are implied indicators. The adoption and correct application of these methods and technologies reflect an upgraded technological capability and innovation within the industry (Target 9.5).
Summary Table
| SDGs | Targets | Indicators |
|---|---|---|
| SDG 3: Good Health and Well-being | 3.d: Strengthen capacity for health risk reduction and management. |
|
| SDG 9: Industry, Innovation, and Infrastructure |
9.1: Develop quality, reliable, and resilient infrastructure.
9.5: Enhance scientific research and upgrade technological capabilities. |
|
Source: meddeviceonline.com