Report on the Epidemiology of Severe Mycoplasma Pneumoniae and its Correlation with Environmental Pollutants (2020-2023)
Executive Summary
This report details a retrospective analysis of severe Mycoplasma pneumoniae (MP) cases in the Pediatric Intensive Care Unit (PICU) of Hunan Children’s Hospital from 2020 to 2023. The study investigates epidemiological patterns and the correlation between disease incidence and atmospheric pollutants. The findings provide critical evidence for public health strategies aligned with the United Nations Sustainable Development Goals (SDGs), particularly SDG 3 (Good Health and Well-being) and SDG 11 (Sustainable Cities and Communities). The overall MP-IgM positivity rate among 2,047 children with severe pneumonia was 9.5%, with a significant increasing trend from 6.3% in 2020 to 15.7% in 2023. Preschool children (3–7 years) and the summer season were identified as high-risk groups and periods, respectively. Crucially, a moderate positive correlation was found between severe MP cases and concentrations of PM2.5, PM10, and NO2 when levels exceeded established health thresholds, underscoring the direct impact of urban air quality on child health and highlighting the urgency of achieving SDG Target 3.9 (reduce deaths from pollution) and SDG Target 11.6 (improve air quality).
1. Introduction: Pediatric Health and Environmental Sustainability
Severe pneumonia remains a leading cause of mortality in children under five, representing a significant challenge to achieving SDG 3, Target 3.2, which aims to end preventable deaths of newborns and children. Mycoplasma pneumoniae is a major contributor to community-acquired pneumonia, with severe cases requiring intensive care. Understanding the epidemiology of this pathogen is vital for effective prevention and treatment. Furthermore, the interplay between infectious diseases and environmental factors is a critical area of concern for sustainable development. Air pollution, a key focus of SDG 11 (Sustainable Cities and Communities) and SDG 13 (Climate Action), has been identified as a potential exacerbating factor for respiratory infections. This study explores this link by analyzing the correlation between severe MP pneumonia and atmospheric pollutants (PM2.5, PM10, NO2), providing data to inform integrated policies that protect child health and promote environmental sustainability.
2. Methodology
2.1 Study Design and Subjects
- Design: A retrospective analysis was conducted on clinical data from the PICU of Hunan Children’s Hospital.
- Period: January 1, 2020, to December 31, 2023.
- Subjects: 2,047 children diagnosed with severe pneumonia who underwent Mycoplasma antibody testing. Diagnosis of severe MP pneumonia was based on the “Guidelines for the Diagnosis and Treatment of Mycoplasma Pneumoniae Pneumonia in Children (2023 Edition).”
2.2 Data Collection and Analysis
- Clinical Data: MP-IgM antibody positivity rates were compared across different years, seasons, age groups, and sexes. A titer ≥ 1:160 was considered positive.
- Environmental Data: Monthly average concentrations of PM2.5, PM10, and NO2 were obtained from the Changsha Ecological Environment Bureau. Average temperature and humidity data were sourced from World Weather Online.
- Statistical Analysis: SPSS 25.0 and R(4.4.3) were used for analysis. The χ2 test was used for group comparisons. Linear correlation and regression models were employed to assess the relationship between pollutant concentrations and disease incidence, particularly above the following thresholds:
- PM2.5 ≥ 35 µg/m3
- PM10 ≥ 50 µg/m3
- NO2 ≥ 25 µg/m3
3. Key Findings
3.1 Epidemiological Characteristics
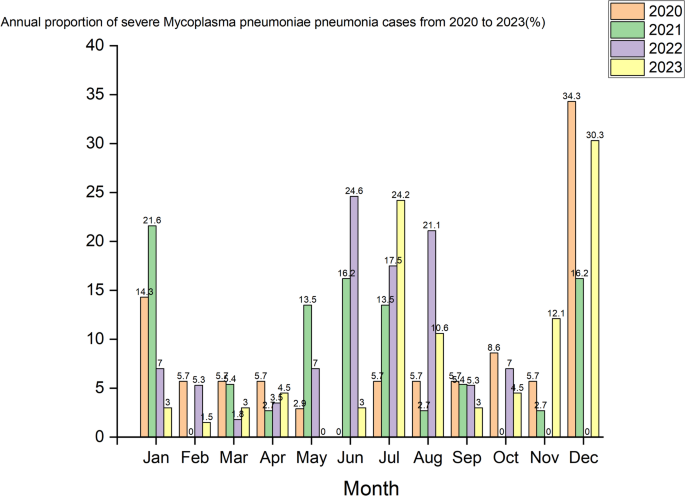
- Annual Trend: The positivity rate of severe MP pneumonia showed a statistically significant increase, rising from 6.3% in 2020 to 15.7% in 2023. This upward trend poses a challenge to progress on SDG 3.
- Seasonal Variation: The highest incidence was recorded in summer (15.8%), which was significantly higher than in other seasons.
- Age Distribution: Preschool children (3–7 years) were the most affected group, with a positivity rate of 30.0%. Infants (<1 year) had the lowest rate (1.6%). This highlights a key vulnerable population for targeted health interventions.
- Sex Distribution: No statistically significant difference was observed between males (8.6%) and females (11.3%).
3.2 Correlation with Environmental Pollutants
A significant positive correlation between air pollutant levels and severe MP cases was observed only when concentrations exceeded established safety thresholds, directly linking poor air quality to adverse child health outcomes as outlined in SDG 3.9.
- PM2.5: At concentrations ≥ 35 µg/m3, a moderate positive correlation was observed (r = 0.40, P < 0.05), with a risk ratio (RR) of 1.28 for every 10 µg/m3 increase.
- PM10: At concentrations ≥ 50 µg/m3, a moderate positive correlation was found (r = 0.41, P < 0.05), with an RR of 1.31 for every 10 µg/m3 increase.
- NO2: At concentrations ≥ 25 µg/m3, a moderate positive correlation was identified (r = 0.47, P < 0.05), with an RR of 2.04 for every 10 µg/m3 increase.
These findings provide compelling evidence that reducing urban air pollution is a critical public health intervention necessary for achieving the goals of SDG 11 and protecting vulnerable pediatric populations.
4. Discussion: Implications for Sustainable Development Goals
4.1 Advancing Child Health (SDG 3)
The increasing prevalence of severe MP pneumonia from 2020 to 2023 underscores a growing public health threat that directly impacts the achievement of SDG 3. The heightened vulnerability of preschool-aged children necessitates targeted prevention strategies, including enhanced surveillance and health education for parents and caregivers. The study demonstrates that environmental health is inseparable from human health; therefore, efforts to reduce child mortality and illness must include measures to mitigate environmental risk factors.
4.2 Building Sustainable and Healthy Cities (SDG 11)
The strong, threshold-dependent correlation between PM2.5, PM10, NO2, and severe pediatric pneumonia provides a clear mandate for action under SDG 11. Achieving Target 11.6, which calls for reducing the adverse environmental impact of cities by improving air quality, is not only an environmental goal but a fundamental requirement for safeguarding public health. The data suggest that policies aimed at reducing traffic and industrial emissions could yield direct and measurable benefits in reducing severe respiratory infections in children, thereby creating healthier and more resilient urban communities.
5. Conclusion and Recommendations
The incidence of severe Mycoplasma pneumoniae pneumonia in the PICU is increasing, with preschool children and the summer season identified as periods of highest risk. More importantly, this study establishes a significant link between elevated levels of key air pollutants (PM2.5, PM10, and NO2) and the burden of severe respiratory disease in children. This connection highlights the urgent need for an integrated approach to public health and environmental policy.
Recommendations for Action
- Strengthen Public Health Surveillance: Enhance monitoring of pediatric respiratory infections to identify trends and vulnerable populations, providing timely data to support the preventative health objectives of SDG 3.
- Implement Strict Air Quality Standards: Policymakers should enforce and strengthen air quality regulations to keep pollutant levels below health-damaging thresholds, directly contributing to SDG 11.6 and SDG 3.9.
- Promote Integrated Urban Planning: Foster urban development that prioritizes public health through green infrastructure, sustainable transport, and reduced industrial emissions, creating cities that are healthy for both people and the planet.
Analysis of Sustainable Development Goals in the Article
1. Which SDGs are addressed or connected to the issues highlighted in the article?
-
SDG 3: Good Health and Well-being
The article’s primary focus is on the health of children, specifically analyzing the epidemiological characteristics of severe Mycoplasma pneumoniae. It directly addresses health outcomes by aiming to “improve clinical outcomes, reducing mortality rates among patients with severe cases.” The investigation into a leading cause of death in children under five (“Severe pneumonia is a leading cause of death in children younger than five years”) firmly connects the research to ensuring healthy lives and promoting well-being for all ages.
-
SDG 11: Sustainable Cities and Communities
The study explicitly links the incidence of severe pneumonia in the Changsha region to urban environmental factors, particularly air pollution. By analyzing the “correlations of PM2.5, PM10, and NO2 concentrations” with the disease, the article addresses the environmental quality and health impacts within a city. This aligns with the goal of making cities and human settlements inclusive, safe, resilient, and sustainable, with a specific focus on air quality management.
2. What specific targets under those SDGs can be identified based on the article’s content?
-
Target 3.2: End preventable deaths of newborns and children under 5 years of age.
The article directly relates to this target by studying a disease that is a “leading cause of death in children younger than five years.” The stated goal of the research is to provide “evidence-based guidance for clinical practice” to ultimately “reduc[e] mortality rates among patients with severe cases.” This demonstrates a clear effort to understand and combat a cause of child mortality.
-
Target 3.9: Substantially reduce the number of deaths and illnesses from hazardous chemicals and air, water and soil pollution and contamination.
This target is central to the article’s hypothesis that “higher pollutant levels would be associated with an increased risk of severe M. pneumoniae pneumonia.” The study investigates the health impacts of air pollutants (PM2.5, PM10, and NO2), finding that at certain concentrations, they are “moderately positively correlated with the number of severe Mycoplasma pneumoniae cases.” This research directly contributes to understanding and quantifying illnesses caused by air pollution.
-
Target 11.6: Reduce the adverse per capita environmental impact of cities, including by paying special attention to air quality.
The article’s methodology relies on monitoring and analyzing urban air quality. It uses “monthly average concentrations of atmospheric pollutants, including PM2.5 (µg/m3), PM10 (µg/m3), and NO2 (µg/m3)” from the Changsha Ecological Environment Bureau. By linking these specific air quality metrics to severe health outcomes in the urban pediatric population, the study underscores the importance of managing and improving city air quality to reduce its adverse environmental and health impacts.
3. Are there any indicators mentioned or implied in the article that can be used to measure progress towards the identified targets?
-
Indicator 3.2.1: Under-5 mortality rate.
While the article does not provide the overall mortality rate, its focus on a “leading cause of death in children younger than five years” and its aim to “reduc[e] mortality rates” implies that the under-5 mortality rate is the ultimate metric of success. The study’s measurement of disease prevalence (“positivity rate of 9.5%”) serves as a proxy indicator for a condition contributing to this mortality rate.
-
Indicator 3.9.1: Mortality rate attributed to household and ambient air pollution.
The article provides direct quantitative data that can be used to assess this indicator. It calculates specific “risk ratios (RR)” for developing severe pneumonia with increased pollutant levels, such as an “RR of 1.28 per 10 µg/m3 increase” for PM2.5 and an “RR of 2.04 per 10 µg/m3 increase” for NO2. These statistics directly measure the health burden attributable to ambient air pollution.
-
Indicator 11.6.2: Annual mean levels of fine particulate matter (e.g. PM2.5 and PM10) in cities.
The article explicitly uses the data that constitutes this indicator. It analyzes the “monthly average concentrations of atmospheric pollutants, including PM2.5 (µg/m3), PM10 (µg/m3), and NO2 (µg/m3).” Furthermore, it uses specific thresholds based on WHO and national standards, such as “PM2.5 ≥ 35 µg/m3” and “PM10 ≥ 50 µg/m3,” which are direct measurements of urban air pollution levels.
4. Summary Table of SDGs, Targets, and Indicators
| SDGs | Targets | Indicators |
|---|---|---|
| SDG 3: Good Health and Well-being | 3.2: End preventable deaths of newborns and children under 5 years of age. | 3.2.1: The article implies the Under-5 mortality rate by studying a “leading cause of death in children younger than five years” and aiming to “reduc[e] mortality rates.” |
| 3.9: Substantially reduce the number of deaths and illnesses from hazardous chemicals and air, water and soil pollution and contamination. | 3.9.1: The article measures the mortality rate attributed to ambient air pollution by calculating risk ratios (e.g., “RR of 1.28, 1.31, and 2.04 per 10 µg/m³ increase” for PM2.5, PM10, and NO2 respectively) linking pollutants to severe illness. | |
| SDG 11: Sustainable Cities and Communities | 11.6: Reduce the adverse per capita environmental impact of cities, including by paying special attention to air quality. | 11.6.2: The study directly uses annual mean levels of fine particulate matter by analyzing “monthly average concentrations of atmospheric pollutants, including PM2.5 (µg/m3), PM10 (µg/m3), and NO2 (µg/m3)” in the city of Changsha. |
Source: nature.com