Report on Novel Coronary Heart Disease Risk Prediction Models and Their Contribution to Sustainable Development Goals
1.0 Introduction: Addressing Non-Communicable Diseases under SDG 3
Coronary Heart Disease (CHD), a leading non-communicable disease (NCD), represents a significant barrier to achieving Sustainable Development Goal 3 (Good Health and Well-being), particularly Target 3.4, which aims to reduce premature mortality from NCDs by one-third by 2030. Current clinical risk prediction tools, such as the Pooled Cohort Equations (PCE) and Systematic COronary Risk Evaluation 2 (SCORE2), rely on laboratory-based markers, limiting their accessibility and scalability, especially in low-resource settings. This creates inequities in preventative care and hampers progress towards universal health coverage (SDG Target 3.8). This report details a study to develop and validate a novel, non-laboratory-based Lifestyle-Based Model (LBM) for CHD risk prediction. By integrating wearable technology and genetic data, this research aligns with SDG 9 (Industry, Innovation, and Infrastructure) to create accessible health solutions that empower individuals and support global public health objectives.
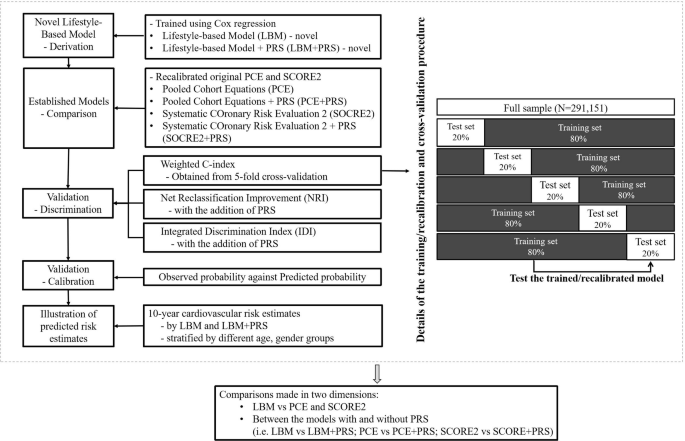
2.0 Methodology
The study utilized a prospective cohort design to develop and validate new CHD risk prediction models, comparing them against established clinical standards.
2.1 Study Population and Data Source
- Data Source: UK Biobank prospective cohort study.
- Participants: 291,151 white British individuals with no history of cardiovascular events at baseline.
- Follow-up: A median of 13.8 years, during which 13,063 incident CHD cases were identified.
2.2 Model Development and Variables
- Lifestyle-Based Model (LBM): Developed using Cox regression with predictors that do not require laboratory testing, promoting accessibility in line with SDG 3.8.
- Age and Sex
- Body Mass Index (BMI)
- Dietary Intake Score (0-3)
- Smoking Status
- Physical Activity (derived from wearable device data)
- Polygenic Risk Score (PRS): A weighted PRS for CHD was calculated based on 300 genetic variants to assess the value of genetic information in risk prediction.
- Established Models for Comparison:
- Pooled Cohort Equations (PCE)
- Systematic COronary Risk Evaluation 2 (SCORE2)
2.3 Performance Evaluation
Model performance was assessed through 5-fold cross-validation, focusing on:
- Discrimination: Measured by the C-index, indicating the model’s ability to distinguish between individuals who will and will not develop CHD.
- Calibration: Assessed using calibration plots and Greenwood-Nam-D’Agostino (GND) tests to evaluate the agreement between predicted and observed risk.
- Risk Reclassification: Evaluated using Net Reclassification Improvement (NRI) and Integrated Discrimination Index (IDI) to determine the added value of incorporating PRS.
3.0 Key Findings
3.1 Predictive Performance of the Lifestyle-Based Model (LBM)
- The LBM demonstrated moderate and comparable predictive accuracy to the established, laboratory-based PCE and SCORE2 models.
- The C-index for the LBM was 0.713, which was similar to the PCE (0.714) and SCORE2 (0.709).
- The LBM showed strong calibration (slope: 0.981; p-value: 0.999), indicating a high degree of accuracy between predicted and observed CHD risk.
3.2 Impact of Integrating Polygenic Risk Scores (PRS)
- Adding PRS significantly improved the discrimination of all models, underscoring the potential of genetic data in enhancing preventative health strategies.
- The C-index for the LBM+PRS increased to 0.733.
- The C-index for PCE+PRS and SCORE2+PRS increased to 0.726 and 0.721, respectively.
- The addition of PRS to the LBM resulted in a positive net reclassification improvement of 4.30%, correctly reclassifying individuals into more accurate risk categories.
4.0 Discussion: Implications for Sustainable Development
4.1 Advancing SDG 3: Good Health and Well-being
The development of the LBM is a critical step towards achieving SDG 3. By providing a tool for CHD risk assessment that is independent of clinical laboratories, the LBM can democratize preventative healthcare.
- Contribution to Target 3.4 (Reduce NCD Mortality): The LBM enables early identification of at-risk individuals through accessible lifestyle metrics. This facilitates timely, low-cost interventions focused on modifiable risk factors like diet and physical activity, directly contributing to the prevention of premature CHD mortality.
- Support for Target 3.8 (Universal Health Coverage): The non-invasive and low-cost nature of the LBM makes it a highly scalable tool for public health screening in diverse settings, including communities with limited access to healthcare facilities. This approach helps reduce health inequities and promotes universal access to preventative services.
4.2 Leveraging Innovation for Global Health (SDG 9)
This study exemplifies the application of innovation (SDG 9) to address pressing health challenges. The integration of data from consumer-grade wearable devices and advanced genetic scoring into a predictive health model showcases a forward-looking approach to public health.
- The use of wearable technology allows for streamlined and continuous data collection, empowering individuals to monitor and manage their own health.
- While PRS integration requires infrastructure, its proven value in improving prediction accuracy points towards future directions for personalized medicine that can further strengthen preventative care systems.
4.3 Limitations and Future Directions for Global Applicability
To maximize the contribution to the global SDG agenda, future work must address the study’s limitations. The model was developed using a white British population, and its external validation across diverse ethnic and socio-economic groups is essential. Future research should focus on recalibrating and validating the LBM in developing countries, where the burden of CHD is rising and the need for accessible, low-cost health solutions is most acute. Such efforts are crucial to ensure the benefits of this innovation are distributed equitably, leaving no one behind.
5.0 Conclusion
The novel Lifestyle-Based Model (LBM) offers an accurate and feasible method for predicting CHD risk, with performance comparable to established clinical models. Its reliance on easily accessible, non-laboratory data presents a significant opportunity to advance global health priorities outlined in the Sustainable Development Goals. By enabling widespread, low-cost risk assessment, the LBM can empower individuals, strengthen preventative health strategies, and contribute meaningfully to the reduction of premature mortality from NCDs (SDG 3.4) and the promotion of universal health coverage (SDG 3.8). The integration of PRS further enhances predictive accuracy, highlighting a promising pathway for more personalized and effective public health interventions.
Analysis of Sustainable Development Goals (SDGs) in the Article
1. Which SDGs are addressed or connected to the issues highlighted in the article?
The primary Sustainable Development Goal (SDG) addressed in the article is:
- SDG 3: Good Health and Well-being
Detailed Explanation:
The article’s central theme is the prediction and prevention of Coronary Heart Disease (CHD), a major non-communicable disease (NCD). This directly aligns with the objective of SDG 3, which is to “ensure healthy lives and promote well-being for all at all ages.” The study focuses on improving health outcomes by developing more accurate and accessible risk prediction models. The introduction explicitly states that CHD is a significant global health issue, accounting for “approximately 33.3% of all-cause mortality and 49.2% of cardiovascular mortality globally,” underscoring its relevance to global health targets.
2. What specific targets under those SDGs can be identified based on the article’s content?
Based on the article’s focus on NCDs, the following specific target under SDG 3 is identified:
- Target 3.4: By 2030, reduce by one-third premature mortality from non-communicable diseases through prevention and treatment and promote mental health and well-being.
Detailed Explanation:
The article is fundamentally about improving the “primary prevention” of CHD. It states, “Accurate assessment of coronary heart disease (CHD) risk is essential for primary prevention as it informs clinical decisions regarding preventive interventions including lifestyle modification and pharmacotherapy.” By developing novel risk prediction models (LBM and LBM+PRS), the study aims to facilitate “pre-emptive identification of individuals at elevated risk of cardiovascular events, allowing for the prompt implementation of preventive measures.” This work directly contributes to the prevention aspect of Target 3.4, aiming to reduce premature deaths from cardiovascular diseases.
3. Are there any indicators mentioned or implied in the article that can be used to measure progress towards the identified targets?
Yes, the article mentions and implies several indicators relevant to Target 3.4.
- Official Indicator (Mentioned):
- Indicator 3.4.1: Mortality rate attributed to cardiovascular disease, cancer, diabetes or chronic respiratory disease.
Explanation: The article directly references the components of this indicator in its introduction by providing statistics on the global mortality burden of cardiovascular disease. The ultimate goal of improving risk prediction is to reduce the incidence and, consequently, the mortality rate from CHD.
- Indicator 3.4.1: Mortality rate attributed to cardiovascular disease, cancer, diabetes or chronic respiratory disease.
- Implied Indicators (Risk Factors used in the LBM):
The article’s “Lifestyle-Based Model (LBM)” is constructed using key modifiable risk factors for NCDs, which serve as implied indicators for prevention efforts under Target 3.4.
- Prevalence of tobacco use: The LBM uses “smoking status (current, previous, never)” as a key predictor. Monitoring and reducing smoking prevalence is a critical measure of progress in NCD prevention.
- Prevalence of insufficient physical activity: The model innovatively uses “physical activity (wrist-worn wearable-device-derived Euclidean Norm Minus One; ENMO).” This highlights the importance of measuring and promoting physical activity to reduce CHD risk.
- Prevalence of unhealthy diet: The model includes a “dietary intake score (0–3; generated based on self-reported food categories),” which serves as a proxy for measuring dietary habits.
- Prevalence of overweight and obesity: The model includes “body mass index (BMI)” as a predictor. BMI is a standard indicator used globally to track overweight and obesity rates, which are major risk factors for CHD.
4. Summary Table of Findings
| SDGs | Targets | Indicators |
|---|---|---|
| SDG 3: Good Health and Well-being | Target 3.4: By 2030, reduce by one-third premature mortality from non-communicable diseases through prevention and treatment and promote mental health and well-being. |
|
Source: nature.com