Report on the Global Burden of Asthma (1990-2021) in the Context of Sustainable Development Goals
1.0 Introduction: Asthma as a Challenge to Global Health and Equality
Analysis of the global asthma burden from 1990 to 2021 reveals significant disparities that impede progress towards Sustainable Development Goal 3 (Good Health and Well-being) and SDG 10 (Reduced Inequalities). While age-standardized rates have shown some decline, the absolute burden of asthma varies dramatically across nations with different Socio-Demographic Index (SDI) levels. This report outlines these variations, identifies key risk factors linked to multiple SDGs, and proposes strategies to create a more equitable and effective global response.
2.0 Regional Disparities and Universal Health Coverage (SDG 3.8)
The data indicates a clear divergence in asthma outcomes between high-income and low- and middle-income countries (LMICs), highlighting a critical gap in achieving universal health coverage.
2.1 High-Income (High SDI) Regions
- Exhibit the highest age-standardized prevalence and incidence rates of asthma.
- Maintain relatively low age-standardized mortality rates.
- This paradox is attributed to effective asthma management, including access to medications and standardized care, which aligns with the principles of SDG 3.
2.2 Low- and Middle-Income (Low SDI) Regions
- Show lower age-standardized prevalence rates but disproportionately higher age-standardized mortality rates.
- Face significant challenges in accessing effective, available, and affordable medications, a direct barrier to SDG 3.8.
- Lack established long-term medical care standards and suffer from a scarcity of specialized healthcare professionals and organizations, leading to preventable deaths and exacerbating inequalities as outlined in SDG 10.
- African nations, in particular, exemplify the challenges in low-SDI countries, where insufficient healthcare capacity and resources lead to inadequate diagnosis and treatment.
3.0 Risk Factors and Their Intersection with Sustainable Development
The global burden of asthma is driven by multiple risk factors that are intrinsically linked to broader development challenges, requiring a multi-sectoral approach consistent with the SDG framework.
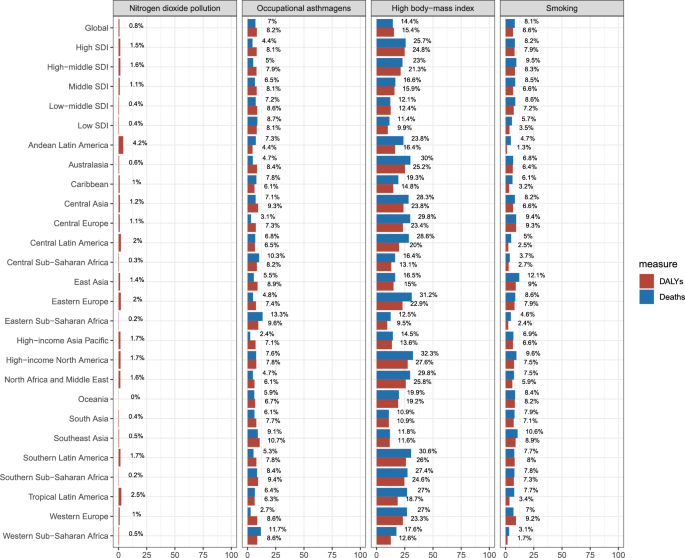
3.1 Key Attributable Risk Factors
- High Body-Mass Index (BMI): A critical contributor to disability-adjusted life years (DALYs), linked to the rise of unhealthy diets and fast foods in nations undergoing economic growth. This challenge intersects with SDG 2 (Zero Hunger), which aims to end all forms of malnutrition, and SDG 3.
- Smoking: A major risk factor for asthma incidence, mortality, and DALYs. Addressing this aligns with public health targets under SDG 3.
- Occupational Asthmagens: Exposure to dust, gases, and chemicals in the workplace contributes significantly to the asthma burden, underscoring the need to ensure safe working environments as per SDG 8 (Decent Work and Economic Growth).
- Nitrogen Dioxide (NO₂) Pollution: A common air pollutant from urbanization, vehicle exhaust, and industrial emissions. This factor directly relates to SDG 11 (Sustainable Cities and Communities) and its goal to reduce the adverse per capita environmental impact of cities.
3.2 Vulnerable Populations
Minors and children experience the highest burden of asthma, including the highest prevalence, incidence, mortality, and DALY rates. Protecting this demographic is essential for achieving the health targets of SDG 3 and ensuring a healthy future generation.
4.0 Strategic Recommendations for an SDG-Aligned Response
A multimodal strategy is required to address the identified risk factors and reduce the global asthma burden, with targeted actions tailored to different development contexts.
4.1 Strengthening Health Systems and Ensuring Access (SDG 3, SDG 10)
- Integrate asthma evaluation and management into primary care to facilitate early detection and treatment of modifiable risk factors.
- Strengthen asthma surveillance systems globally, particularly in LMICs, to inform targeted public health policies.
- Improve the accessibility, quality, and affordability of essential asthma medications and medical resources in LMICs to reduce preventable mortality and close the inequality gap.
4.2 Addressing Environmental and Lifestyle Determinants
- Promote Healthy Diets (SDG 2, SDG 3): Develop culturally relevant dietary standards and promote healthier eating habits to halt the rise in obesity.
- Enhance Tobacco Control (SDG 3): Strengthen tobacco control efforts in LMICs through increased taxes, comprehensive smoke-free regulations, and cessation programs.
- Improve Air Quality and Urban Environments (SDG 11): Reduce air pollution by investing in sustainable energy, improving public transportation, and tightening industrial emission regulations.
- Ensure Workplace Safety (SDG 8): Improve measures to prevent exposure to occupational asthmagens.
5.0 Conclusion: The Imperative for Integrated Action
The global burden of asthma remains a significant public health challenge marked by profound inequalities. The findings underscore the necessity of targeted prevention and treatment initiatives that are aligned with the Sustainable Development Goals. Addressing the asthma burden requires a holistic approach that not only strengthens health systems (SDG 3) but also tackles underlying determinants related to nutrition (SDG 2), decent work (SDG 8), and sustainable cities (SDG 11). Reducing these inequalities (SDG 10) is fundamental to ensuring good health and well-being for all populations.
Analysis of Sustainable Development Goals in the Article
1. Which SDGs are addressed or connected to the issues highlighted in the article?
-
SDG 3: Good Health and Well-being
This is the primary SDG addressed, as the entire article focuses on the global burden of asthma, a chronic respiratory disease. It discusses prevalence, mortality rates, risk factors, and disparities in healthcare access and quality, all of which are central to ensuring healthy lives and promoting well-being.
-
SDG 10: Reduced Inequalities
The article explicitly highlights significant disparities between high-income countries and low- and middle-income countries (LMICs). It notes that while prevalence may be high in wealthy nations, mortality is low due to effective management, whereas in LMICs, “although the age-standardized prevalence of asthma is lower, the age-standardized mortality rate is higher.” This directly points to inequalities in health outcomes and access to healthcare resources among countries.
-
SDG 11: Sustainable Cities and Communities
The article connects the burden of asthma to environmental factors prevalent in urban settings. It mentions “urbanization” as an unavoidable risk factor and identifies “Nitrogen dioxide pollution,” which primarily comes from “vehicle exhaust and industrial emissions,” as a significant contributor to the global burden of asthma. This relates to the goal of reducing the adverse environmental impact of cities, particularly concerning air quality.
-
SDG 8: Decent Work and Economic Growth
The analysis of risk factors identifies “Occupational asthmagens” as a substantial contributor to the burden of asthma and Disability-Adjusted Life Years (DALYs). This connects the issue to the need for safe and secure working environments, a key component of decent work.
2. What specific targets under those SDGs can be identified based on the article’s content?
-
Under SDG 3: Good Health and Well-being
- Target 3.4: By 2030, reduce by one-third premature mortality from non-communicable diseases through prevention and treatment. The article directly addresses this by analyzing the “age-standardized mortality rate” for asthma (a non-communicable disease) and discussing how “unnecessary deaths” could be prevented through better treatment and management of risk factors.
- Target 3.8: Achieve universal health coverage, including access to quality essential health-care services and access to safe, effective, quality and affordable essential medicines. The article highlights the failure to meet this target in LMICs, stating that “accessing effective, available, and affordable medications presents a significant challenge” and there is a “scarcity of outstanding doctors and specialized organizations.”
- Target 3.9: By 2030, substantially reduce the number of deaths and illnesses from hazardous chemicals and air, water and soil pollution and contamination. The identification of “Nitrogen dioxide pollution” as a key risk factor for asthma directly links the disease burden to air pollution, aligning with this target.
- Target 3.a: Strengthen the implementation of the World Health Organization Framework Convention on Tobacco Control. The article identifies “Smoking” as a major risk factor for asthma DALYs and recommends strengthening “tobacco control efforts” as a key strategy to reduce the disease burden.
-
Under SDG 10: Reduced Inequalities
- Target 10.2: By 2030, empower and promote the social, economic and political inclusion of all, irrespective of… economic or other status. The article’s core finding is the disparity in health outcomes based on a country’s Socio-Demographic Index (SDI). The higher mortality in low-SDI countries despite lower prevalence demonstrates a clear inequality in access to life-saving healthcare, which is a form of exclusion based on economic status.
-
Under SDG 11: Sustainable Cities and Communities
- Target 11.6: By 2030, reduce the adverse per capita environmental impact of cities, including by paying special attention to air quality. The article’s emphasis on “Nitrogen dioxide pollution” from “vehicle exhaust and industrial emissions” as a cause of asthma directly supports the need to improve urban air quality as outlined in this target.
-
Under SDG 8: Decent Work and Economic Growth
- Target 8.8: Protect labour rights and promote safe and secure working environments for all workers. The article’s finding that “Occupational asthmagens” are a significant risk factor for asthma highlights the importance of workplace safety in preventing chronic disease, which is central to this target.
3. Are there any indicators mentioned or implied in the article that can be used to measure progress towards the identified targets?
-
Indicators for SDG 3 Targets
- For Target 3.4: The article explicitly uses metrics that align with Indicator 3.4.1 (Mortality rate attributed to cardiovascular disease, cancer, diabetes or chronic respiratory disease). It repeatedly refers to the “age-standardized mortality rate” (ASDR) and “Disability-Adjusted Life Years” (DALYs) for asthma, which are direct measures of the burden of a chronic respiratory disease.
- For Target 3.8: While not citing a specific indicator number, the article implies the need for indicators related to universal health coverage. The statement about the challenge in “accessing effective, available, and affordable medications” points to an indicator like the proportion of the population with access to affordable essential medicines. The mention of a “scarcity of outstanding doctors” implies an indicator like health worker density.
- For Target 3.9: The article’s focus on “Nitrogen dioxide pollution” as a risk factor relates to Indicator 3.9.1 (Mortality rate attributed to household and ambient air pollution). The burden of asthma caused by air pollution is a component of the overall illness and death attributable to this environmental hazard.
- For Target 3.a: The identification of “Smoking” as a major risk factor directly relates to Indicator 3.a.1 (Age-standardized prevalence of current tobacco use). Reducing the prevalence of smoking is the primary goal of tobacco control efforts mentioned in the article.
-
Indicators for Other SDG Targets
- For Target 11.6: The mention of “Nitrogen dioxide pollution” relates to Indicator 11.6.2 (Annual mean levels of fine particulate matter (e.g. PM2.5 and PM10) in cities). NO₂ is a key indicator of urban air pollution, often measured alongside particulate matter to assess the environmental impact of cities.
- For Target 8.8: The discussion of “Occupational asthmagens” implies the need for indicators related to Indicator 8.8.1 (Frequency rates of fatal and non-fatal occupational injuries and diseases). The burden of asthma attributable to occupational exposure is a measure of non-fatal occupational disease.
- Implied Indicator for Nutrition (related to SDG 2): The article identifies “High body-mass index” as the most critical risk factor for DALYs. This directly relates to indicators of malnutrition and obesity, such as Indicator 2.2.2 (Prevalence of malnutrition… by type (wasting and overweight)).
4. Summary Table of SDGs, Targets, and Indicators
| SDGs | Targets | Indicators Identified or Implied in the Article |
|---|---|---|
| SDG 3: Good Health and Well-being |
3.4: Reduce premature mortality from non-communicable diseases.
3.8: Achieve universal health coverage and access to affordable essential medicines. 3.9: Reduce deaths and illnesses from air pollution. 3.a: Strengthen tobacco control. |
Indicator 3.4.1: The article directly measures and discusses the “age-standardized mortality rate” and “Disability-Adjusted Life Years (DALYs)” for asthma.
Implied Indicator: The article implies indicators on access to medicines and healthcare professionals by highlighting the “challenge” in accessing “affordable medications” and the “scarcity of outstanding doctors” in LMICs. Indicator 3.9.1: The article links the asthma burden to “Nitrogen dioxide pollution,” which is a component of ambient air pollution measured by this indicator. Indicator 3.a.1: The article identifies “Smoking” as a key risk factor, directly relating to the prevalence of tobacco use. |
| SDG 10: Reduced Inequalities | 10.2: Promote inclusion of all, irrespective of economic or other status. | Implied Indicator: The article’s comparison of mortality and prevalence rates between high and low Socio-Demographic Index (SDI) regions serves as a measure of health inequality. |
| SDG 11: Sustainable Cities and Communities | 11.6: Reduce the adverse per capita environmental impact of cities, especially air quality. | Indicator 11.6.2: The focus on “Nitrogen dioxide pollution” from urban sources like “vehicle exhaust” directly relates to the measurement of annual mean levels of urban air pollutants. |
| SDG 8: Decent Work and Economic Growth | 8.8: Promote safe and secure working environments. | Indicator 8.8.1: The identification of “Occupational asthmagens” as a major risk factor points to the need to measure the frequency of occupational diseases. |
| (Related) SDG 2: Zero Hunger | 2.2: End all forms of malnutrition. | Indicator 2.2.2: The article identifies “High body-mass index” and obesity as the most critical risk factor, which is measured by indicators of overweight/obesity prevalence. |
Source: bmcpulmmed.biomedcentral.com