Advancements in Male Contraception and Alignment with Sustainable Development Goals
Research and development in male contraception are advancing, presenting a critical opportunity to progress towards key Sustainable Development Goals (SDGs). The expansion of contraceptive options to include men directly supports SDG 3 (Good Health and Well-being) by promoting universal access to sexual and reproductive healthcare services. Furthermore, it is integral to achieving SDG 5 (Gender Equality) by fostering shared responsibility in family planning and empowering individuals with greater control over their reproductive health.
Societal Shifts and Demand for Gender Equality in Family Planning
A notable shift in societal attitudes is driving the demand for male contraceptive methods. The historical burden of contraception has predominantly been placed on women, a situation increasingly viewed as a constraint. Public skepticism towards female hormonal methods has amplified calls for new alternatives that enhance safety and choice, aligning with the objectives of SDG 3. Concurrently, the movement for gender equality has spurred advocacy for men to assume an active role in contraceptive responsibility. This cultural evolution is essential for fulfilling the targets of SDG 5, which call for the equal sharing of responsibilities within households and families.
Analysis of Male Contraceptive Methods in Development
Several methods are in various stages of development, ranging from hormonal to reversible surgical options. These innovations promise to diversify the contraceptive landscape, contributing to improved global health outcomes.
Hormonal Contraception
Hormonal methods represent one of the most advanced areas of research, with studies indicating high potential user acceptance (44%-83%).
- Transdermal Gel: A combination of nestorone (progestin) and testosterone is in late-stage clinical trials. The progestin component blocks sperm production, while testosterone is administered at a replacement dose to maintain normal physiological functions and mitigate side effects.
- Oral Formulations: Development of oral options is focused on molecules like 11-beta-MNTDC and dimethandrolone, as oral testosterone is limited by poor bioavailability.
- Efficacy and Side Effects: These methods require approximately six months to become fully effective. Potential side effects are similar to those experienced by women, including acne, weight changes, altered libido, and mood fluctuations.
Non-Hormonal Contraception
Non-hormonal approaches target alternative biological pathways to avoid the side effects associated with hormonal manipulation.
- Retinoic Acid Antagonists: This strategy focuses on disrupting spermatogenesis, which is dependent on retinoic acid (a metabolite of Vitamin A).
- YCT-529: The most advanced candidate is an oral selective retinoic acid receptor-alpha antagonist. Studies in nonhuman primates have demonstrated its ability to induce reversible seminiferous tubule hypoplasia, with fertility restored after treatment cessation.
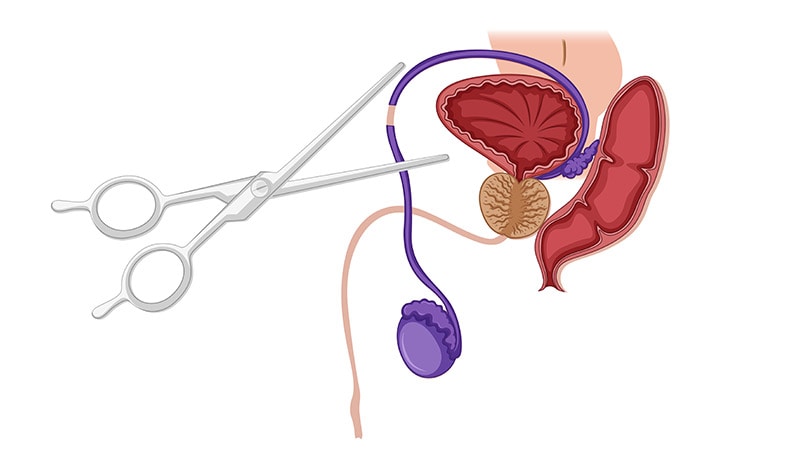
Surgical and Long-Acting Reversible Methods
Current and emerging procedures offer long-term or permanent solutions, with a growing focus on reversibility to meet diverse family planning needs.
- Vasectomy: A permanent surgical procedure that has seen a significant increase in popularity, with a 491% rise in France between 2010 and 2018. Due to its irreversibility, it is subject to strict legal regulation.
- Vasalgel: A polymer gel injected into the vas deferens that provides contraception for approximately 14 months. It is designed to be reversible with a sodium bicarbonate injection, although complete restoration of sperm morphology remains a research focus.
- Implantable Microswitch: An “on-demand vasectomy” concept is in development. This device would be implanted near the vas deferens and could be activated or deactivated externally to block or permit sperm passage.
Thermal Methods
This approach involves temporarily reducing sperm production by maintaining testicular temperature above 35°C for extended periods using specialized undergarments. The market availability of devices like the Andro-switch ring is currently pending regulatory certification.
Barriers to Implementation and Future Outlook
Despite scientific progress, significant obstacles hinder the widespread availability and adoption of male contraception. Overcoming these challenges is crucial for realizing the full potential of these advancements in contributing to SDGs 3 and 5.
- Pharmaceutical Investment: There is limited interest and investment from the pharmaceutical industry, slowing research and commercialization.
- Societal and Cultural Norms: Deep-seated attitudes regarding masculinity and traditional gender roles may impede adoption.
- Interpersonal Trust: Questions remain regarding whether women are prepared to trust male partners with the responsibility of contraception, given the potential consequences of noncompliance.
Analysis of SDGs, Targets, and Indicators
1. Which SDGs are addressed or connected to the issues highlighted in the article?
-
SDG 3: Good Health and Well-being
- The article’s central theme is the development of new male contraceptive methods. Contraception is a fundamental component of sexual and reproductive health, which is a key area of focus for SDG 3. The text discusses various hormonal, non-hormonal, and surgical options aimed at improving family planning choices and overall well-being.
-
SDG 5: Gender Equality
- The article explicitly links the development of male contraception to the broader push for gender equality. It highlights the “growing demand for men to take a more active role in family planning and share contraceptive responsibility,” which directly addresses the goal of achieving gender equality and empowering all women and girls by distributing the responsibility of family planning more evenly between partners.
2. What specific targets under those SDGs can be identified based on the article’s content?
-
Target 3.7: By 2030, ensure universal access to sexual and reproductive health-care services, including for family planning, information and education, and the integration of reproductive health into national strategies and programmes.
- The development of new male contraceptives, such as the transdermal gel, oral pills (YCT-529), and reversible surgical methods (Vasalgel), directly contributes to this target by expanding the range of available family planning methods. The article discusses the need for “reliable, reversible, and accessible male contraceptive methods,” which aligns with the goal of ensuring universal access to comprehensive family planning services.
-
Target 5.6: Ensure universal access to sexual and reproductive health and reproductive rights as agreed in accordance with the Programme of Action of the International Conference on Population and Development and the Beijing Platform for Action and the outcome documents of their review conferences.
- This target is addressed through the article’s emphasis on shared responsibility and choice. By creating more contraceptive options for men, the burden of family planning, which has historically fallen on women, can be shared. The article notes that female contraception is “now sometimes experienced as a constraint by women,” and the push for male options reflects a demand for greater equality in reproductive health decisions and rights.
3. Are there any indicators mentioned or implied in the article that can be used to measure progress towards the identified targets?
-
Indicator of Acceptance and Demand for Male Contraception
- The article provides a statistic that can serve as an indicator of public readiness and demand for new family planning methods. It states that “Studies have indicated that 44%-83% of men support male contraception.” This percentage can be used to measure societal attitudes and the potential uptake of new methods, which is crucial for achieving universal access.
-
Indicator of Uptake of Existing Male Contraceptive Methods
- The article provides specific data on the use of vasectomy in France, which can be used as a direct indicator of the use of modern contraceptive methods by men. It states that “procedures in France rose by 491% between 2010 and 2018, with nearly 20,000 operations performed in 2018.” This data point measures the current rate of adoption of a permanent male contraceptive method.
Summary Table of Findings
| SDGs | Targets | Indicators |
|---|---|---|
| SDG 3: Good Health and Well-being | Target 3.7: Ensure universal access to sexual and reproductive health-care services, including for family planning. | The increase in vasectomy procedures in France (a 491% rise between 2010 and 2018) as a measure of the uptake of male contraceptive methods. |
| SDG 5: Gender Equality | Target 5.6: Ensure universal access to sexual and reproductive health and reproductive rights. | The percentage of men willing to use male contraception (cited as 44%-83% in studies) as an indicator of shifting attitudes towards shared contraceptive responsibility. |
Source: medscape.com