Report on Sudden Cardiac Death in Heart Failure with Preserved Ejection Fraction: Aligning Clinical Research with Sustainable Development Goal 3
Introduction: Addressing Non-Communicable Diseases under SDG 3
Heart failure (HF) represents a significant global health challenge, undermining progress towards Sustainable Development Goal 3 (Good Health and Well-being), particularly Target 3.4, which aims to reduce premature mortality from non-communicable diseases (NCDs). Sudden cardiac death (SCD) is a primary contributor to mortality in HF patients. While extensive research exists for HF with reduced ejection fraction (HFrEF), a critical knowledge gap persists for HF with preserved ejection fraction (HFpEF), a phenotype of growing prevalence due to global aging and rising rates of comorbidities like hypertension and diabetes. This lack of understanding impedes the development of effective, targeted interventions necessary to achieve universal health coverage and reduce NCD mortality. This report details a prospective study designed to characterize the incidence, mechanisms, and predictors of SCD in HFpEF, providing crucial evidence to inform public health strategies and advance the objectives of SDG 3.
Methodology for Evidence-Based Health Interventions
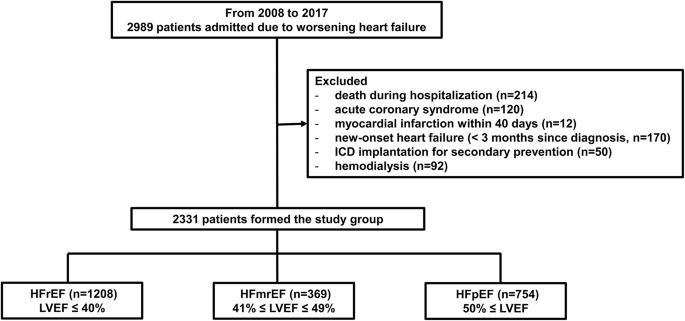
A prospective observational study was conducted to generate robust data for improving health outcomes, a core tenet of SDG 3. The study enrolled 2,331 patients hospitalized for decompensated heart failure.
Study Design and Population
- Cohort Size: 2,331 patients.
- Stratification: Patients were categorized based on left ventricular ejection fraction (LVEF) into three distinct phenotypes:
- Heart Failure with preserved Ejection Fraction (HFpEF): 754 patients
- Heart Failure with mid-range Ejection Fraction (HFmrEF): 369 patients
- Heart Failure with reduced Ejection Fraction (HFrEF): 1,208 patients
- Follow-up Period: A median of 25 months.
- Primary Endpoint: The primary outcome was SCD, with non-SCD death treated as a competing risk to ensure analytical precision.
Statistical Analysis
To ensure the reliability of findings for clinical and public health application, multivariate competing risk analysis was employed. This included cause-specific Cox proportional hazards models and Fine–Gray subdistribution hazard models to identify independent predictors of SCD. This rigorous approach supports the development of evidence-based guidelines essential for strengthening health systems as outlined in SDG 3.
Key Findings: Differentiating Mortality Patterns for Targeted Care
Over the follow-up period, 298 patients (12.8%) experienced SCD. The results revealed significant distinctions across HF phenotypes, highlighting the need for tailored, rather than one-size-fits-all, prevention strategies to effectively reduce premature mortality from NCDs (SDG Target 3.4).
SCD Incidence Across Heart Failure Phenotypes
- HFpEF: Exhibited the lowest incidence of SCD at 5.9%. Non-cardiac causes were the predominant mode of death (45%), underscoring the importance of comprehensive comorbidity management.
- HFmrEF: Demonstrated a higher SCD incidence of 13.8%.
- HFrEF: Showed the highest SCD incidence at 16.7%.
Mechanisms of Sudden Cardiac Death
The underlying mechanisms of SCD varied significantly, indicating different pathophysiological pathways that require distinct clinical approaches.
- In HFpEF, asystole was the predominant mode of SCD, accounting for 52.9% of cases.
- In HFmrEF and HFrEF, ventricular tachyarrhythmias were the dominant mechanism.
This finding is critical for achieving SDG 3, as it suggests that interventions like implantable cardioverter-defibrillators (ICDs), which primarily target tachyarrhythmias, may have limited efficacy in the HFpEF population, necessitating research into alternative preventive measures.
Independent Predictors of SCD in HFpEF
The multivariate competing risk analysis identified two key independent predictors for SCD in the HFpEF cohort. These findings are vital for developing risk stratification tools that enable early warning and risk reduction, contributing to SDG Target 3.d.
- NYHA Class III: Patients with more severe symptoms had a significantly higher risk of SCD (csHR 2.04; sHR 1.56).
- Prolonged QTc Interval (>480 ms): This electrocardiographic marker was a strong independent predictor of SCD (csHR 1.63; sHR 1.57).
Conclusion: Advancing SDG 3 Through Phenotype-Specific Risk Stratification
This study provides definitive evidence that patients with HFpEF have distinct mortality patterns and SCD mechanisms compared to other HF phenotypes. The lower incidence of SCD, the predominance of asystole, and the high rate of non-cardiac death necessitate a paradigm shift in clinical management. Identifying NYHA functional class and the QTc interval as independent predictors offers a tangible pathway toward improved, cost-effective risk stratification. By integrating these findings into clinical practice, healthcare systems can develop targeted prevention strategies for the HFpEF population, directly supporting the global effort to reduce premature mortality from NCDs and achieve the health-related targets of the 2030 Agenda for Sustainable Development.
1. Relevant Sustainable Development Goals (SDGs)
-
SDG 3: Good Health and Well-being
The article’s entire focus is on understanding and addressing a major global health issue: mortality from heart failure (HF) and sudden cardiac death (SCD). It investigates the causes, mechanisms, and predictors of death in different patient populations. This research directly contributes to the overarching goal of ensuring healthy lives and promoting well-being for all at all ages by seeking to improve clinical outcomes for patients with non-communicable diseases.
2. Specific SDG Targets Identified
-
Target 3.4: Reduce premature mortality from non-communicable diseases
This target aims to “reduce by one third premature mortality from non-communicable diseases through prevention and treatment.” Heart failure is a primary non-communicable disease (NCD) and a leading cause of death globally. The article directly addresses this target by analyzing mortality patterns and seeking to identify high-risk patients to “develop precision management strategies.” The study’s findings on predictors of SCD are a crucial step toward creating targeted prevention and treatment plans to reduce deaths from this condition. The introduction states, “Heart failure (HF) is a leading global cause of morbidity and mortality,” highlighting the relevance of this research to the target.
-
Target 3.d: Strengthen capacity for early warning, risk reduction, and management of health risks
The article’s objective is to “enhance risk stratification” for SCD in patients with a specific type of heart failure (HFpEF). By identifying reliable predictors, the study contributes to the capacity for early warning and risk reduction. The conclusion emphasizes that the findings highlight “their potential for risk stratification” and the need for “phenotype-specific strategies.” This work provides clinicians with better tools to manage the health risks associated with heart failure, directly aligning with the goal of strengthening national and global health risk management capacities.
3. Indicators for Measuring Progress
-
Indicator 3.4.1: Mortality rate attributed to cardiovascular disease, cancer, diabetes or chronic respiratory disease
The article provides precise data that can be used for this indicator. It measures mortality from cardiovascular disease within a specific cohort. Specific data points include:
- Overall mortality: “During the median follow-up period of 25 months, 909 (38.9%) patients died.”
- SCD-specific mortality: “298 (12.8%) patients developed SCD.”
- Mortality rates by disease phenotype: The study reports the incidence of SCD as 5.9% in HFpEF patients, 13.8% in HFmrEF patients, and 16.7% in HFrEF patients. This detailed data is essential for tracking mortality rates attributed to cardiovascular disease.
-
Implied Indicators for Risk Stratification (related to Target 3.d)
The article does not mention official UN indicators for Target 3.d, but it identifies specific clinical markers that serve as practical, measurable indicators for risk stratification and management capacity. These are the tools that enable progress towards the target.
- NYHA (New York Heart Association) functional class: The study found that “NYHA functional class III” was an independent predictor of SCD in HFpEF patients. The proportion of high-risk patients identified by this class can be used as an indicator to measure the effectiveness of risk management strategies.
- QTc interval: The research identified a “prolonged QTc interval > 480 ms” as another key predictor of SCD. This electrocardiographic measurement is a specific, quantifiable indicator that can be used in clinical practice to identify patients needing targeted interventions, thereby measuring the capacity for early warning and risk reduction.
4. Summary Table of SDGs, Targets, and Indicators
| SDGs | Targets | Indicators |
|---|---|---|
| SDG 3: Good Health and Well-being | 3.4: Reduce by one third premature mortality from non-communicable diseases through prevention and treatment. |
3.4.1: Mortality rate attributed to cardiovascular disease.
|
| SDG 3: Good Health and Well-being | 3.d: Strengthen the capacity of all countries… for early warning, risk reduction and management of national and global health risks. |
Implied Clinical Indicators for Risk Stratification:
|
Source: nature.com