Report on SARS-CoV-2 Contamination in Dental Clinical Environments
Executive Summary
This report details a study investigating the presence and cross-contamination risk of SARS-CoV-2 in restorative dental clinics, a setting characterized by high aerosol generation. The study’s findings underscore critical challenges and opportunities related to achieving Sustainable Development Goal 3 (Good Health and Well-being) and SDG 8 (Decent Work and Economic Growth) by highlighting the necessity of robust infection control and occupational safety protocols. Saliva and environmental samples were analyzed, revealing viral presence even in the absence of patient symptoms, which points to a significant risk of transmission. The report concludes that current disinfection procedures may be inadequate and recommends the development of updated, evidence-based protocols to ensure the safety of patients and healthcare workers, thereby contributing to resilient and sustainable health systems.
1.0 Introduction
The COVID-19 pandemic has presented unprecedented challenges to global health systems, directly impacting the progress toward SDG 3 (Good Health and Well-being). Dental professionals are at an elevated risk of exposure to SARS-CoV-2 due to the nature of their work, which involves aerosol-generating procedures in close proximity to the oral cavity. The potential for airborne transmission in clinical settings threatens not only patient health but also the occupational safety of healthcare workers, a key component of SDG 8 (Decent Work and Economic Growth). This study was initiated to assess the SARS-CoV-2 viral load on patients and environmental surfaces within restorative dental clinics to evaluate the efficacy of existing disinfection protocols and control the spread of infection.
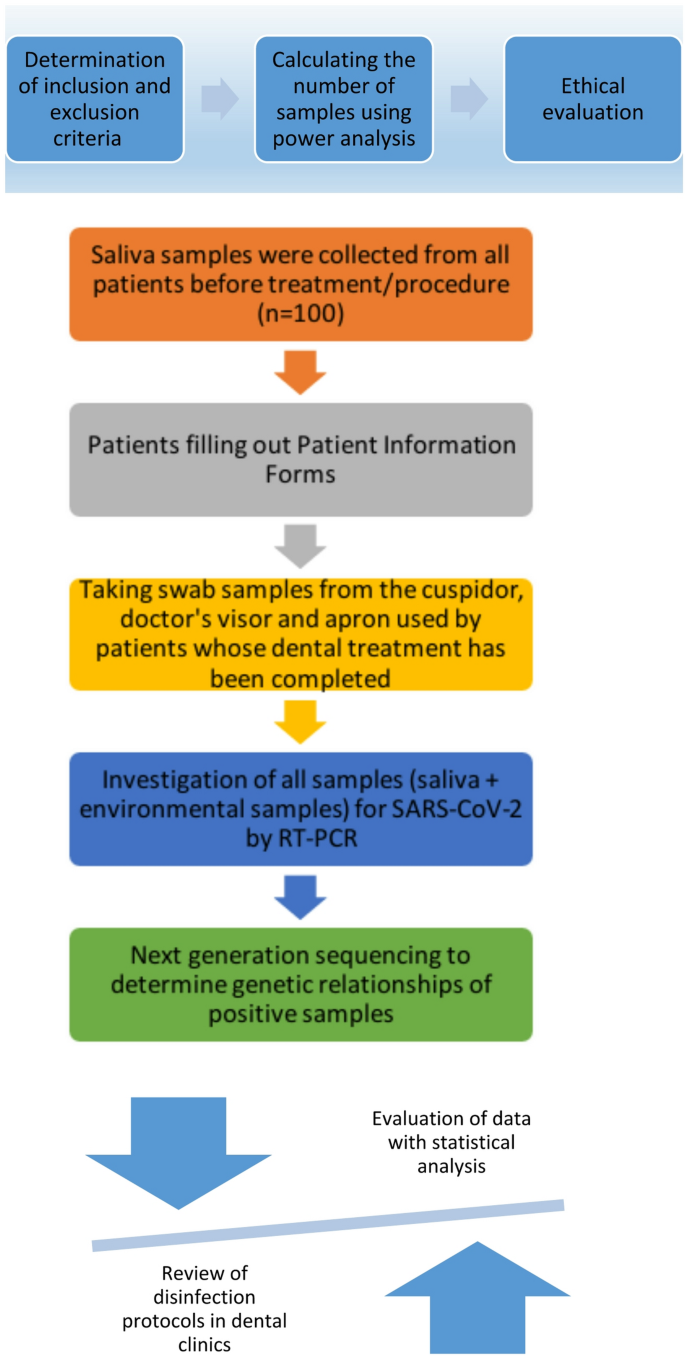
2.0 Methodology
The study was conducted in accordance with established ethical guidelines and received approval from the Erciyes University Clinical Research Ethics Committee. A total of 100 patients and 300 associated environmental samples were included.
2.1 Sample Collection and Participants
- Participants: 100 patients (69 female, 31 male, average age 29.85) voluntarily participated in the study at a restorative dental clinic.
- Patient Samples: Saliva samples were collected from each patient before their dental procedure.
- Environmental Samples: Swabs were taken from three surfaces for each patient post-procedure: the cuspidor (spittoon), the dentist’s visor, and the cuffs of the dentist’s gown.
- Data Collection: Participants completed an information form detailing demographic data, COVID-19 history, contact status, symptoms, and vaccination status.
2.2 Laboratory Analysis
- Viral RNA was isolated from all saliva and environmental samples.
- Qualitative detection of SARS-CoV-2 specific genes (ORF1ab and N) was performed using the quantitative reverse transcription-polymerase chain reaction (qRT-PCR) method.
- Cycle threshold (Ct) values were determined for all positive samples to estimate viral load.
- Next-generation sequencing was planned for positive samples to analyze viral origins, though this was impeded by RNA degradation.
3.0 Key Findings
The analysis yielded positive SARS-CoV-2 RNA results in both patient and environmental samples, indicating active viral shedding and environmental contamination.
3.1 SARS-CoV-2 Positivity Rates
- Patient Samples: 3% (3 out of 100) of patient saliva samples tested positive for SARS-CoV-2 RNA.
- Environmental Samples: 1.3% (4 out of 300) of environmental samples tested positive. These included:
- Two gown cuffs
- One cuspidor
- One visor
- Viral Load: The mean Cycle threshold (Ct) value was 28.2 in patients and 26.9 in environmental samples, suggesting a moderate to significant viral load capable of transmission.
3.2 Correlation with Patient Data
- A statistically significant relationship (p < 0.001) was found between a positive saliva sample and a patient's recent history of COVID-19 infection or close contact with a positive case.
- No significant relationship was observed between SARS-CoV-2 positivity and the presence of chronic diseases.
- Of the patients with positive saliva samples, all had received at least three doses of a COVID-19 vaccine, indicating the potential for breakthrough infections.
4.0 Discussion and Implications for Sustainable Development Goals
The study’s results have significant implications for public health policy and clinical practice, particularly in the context of the UN Sustainable Development Goals.
4.1 SDG 3: Good Health and Well-being
The detection of SARS-CoV-2 in asymptomatic patients and on clinical surfaces highlights a persistent risk of infectious disease transmission. This directly challenges Target 3.d, which calls for strengthening the capacity for early warning, risk reduction, and management of national and global health risks. The findings demonstrate that routine dental procedures can lead to cross-contamination, jeopardizing the health of subsequent patients and staff. The fact that vaccinated individuals can still carry and shed the virus reinforces the need for a multi-layered approach to infection control that does not rely solely on vaccination status. Improving disinfection protocols is essential for safeguarding community health and building resilient healthcare infrastructure.
4.2 SDG 8: Decent Work and Economic Growth
Ensuring a safe working environment is a cornerstone of decent work (Target 8.8). Dental professionals are frontline workers whose health and safety must be protected. The contamination of personal protective equipment (gowns and visors) confirms that healthcare workers are directly exposed to infectious aerosols. Inadequate disinfection measures create an unsafe occupational environment, increasing staff illness, absenteeism, and burnout, which can destabilize the healthcare workforce and economy. By identifying these risks, this study advocates for improved safety standards that protect labor rights and promote productive employment in the healthcare sector.
4.3 SDG 6 & 12: Sustainable Sanitation and Practices
The study implicitly addresses SDG 6 (Clean Water and Sanitation) and SDG 12 (Responsible Consumption and Production) by questioning the efficacy of the disinfectant in use (quaternary ammonium compounds). The persistence of viral RNA suggests that the chosen disinfectant and its application method (spraying) may be insufficient. This calls for a re-evaluation of cleaning agents and protocols. Adopting more effective, evidence-based disinfectants, such as alcohol-based solutions or hypochlorous acid, would improve sanitation standards (SDG 6). Furthermore, selecting appropriate and efficient products and application methods (e.g., wiping vs. spraying) contributes to the responsible use of chemicals and reduces waste, aligning with the principles of sustainable consumption and production (SDG 12).
5.0 Conclusion and Recommendations
This study confirms that aerosol-generating procedures in dental clinics create a tangible risk of SARS-CoV-2 cross-contamination, even from asymptomatic or vaccinated patients. Current disinfection protocols may not be sufficient to mitigate this risk, thereby threatening progress towards key Sustainable Development Goals related to health and occupational safety.
To better align with the objectives of the SDGs, the following actions are recommended:
- Review and Update Disinfection Protocols: Healthcare facilities should transition to disinfectants with proven efficacy against enveloped viruses like SARS-CoV-2 and ensure application methods are consistent with best practices.
- Enhance Occupational Safety Training: Regular training for all clinical staff, including cleaning personnel, on updated sterilization, disinfection, and PPE protocols is crucial for ensuring compliance and effectiveness.
- Promote Continuous Environmental Surveillance: Ongoing monitoring of clinical environments can serve as an early warning system to identify gaps in infection control and prevent outbreaks.
- Strengthen Public Health Integration: Dental clinics should be integrated into broader public health strategies for infectious disease control, ensuring that policies and guidelines reflect the specific risks present in these settings.
1. Which SDGs are addressed or connected to the issues highlighted in the article?
SDG 3: Good Health and Well-being
- The article directly addresses public health by investigating the transmission of a communicable disease, SARS-CoV-2, within a healthcare setting. It focuses on preventing infection, understanding viral spread through aerosols, and managing health risks for both patients and healthcare providers. The discussion on vaccination rates and hesitancy also falls under this goal.
SDG 6: Clean Water and Sanitation
- The study heavily emphasizes the role of hygiene and sanitation in controlling the spread of the virus. It evaluates the effectiveness of existing disinfection procedures and chemicals used for cleaning surfaces in dental clinics, such as cuspidors and visors. The article’s conclusion points to the need for “more accurate disinfectant selection and application methods,” which is central to the hygiene aspect of SDG 6.
SDG 8: Decent Work and Economic Growth
- The article highlights the occupational health and safety of dental professionals. It explicitly states that “Dentists and their assistants are possible targets for SARS-CoV-2” due to their work environment. The investigation into viral contamination on personal protective equipment (gowns, visors) and the overall clinic environment directly relates to ensuring a safe and secure working environment for healthcare workers.
2. What specific targets under those SDGs can be identified based on the article’s content?
SDG 3: Good Health and Well-being
-
Target 3.3: By 2030, end the epidemics of AIDS, tuberculosis, malaria and neglected tropical diseases and combat hepatitis, water-borne diseases and other communicable diseases.
- The entire study is an effort to understand and control the spread of a communicable disease (COVID-19) in a specific high-risk environment. By investigating cross-contamination and aerosol dispersion, the research aims to contribute to methods that can help control the pandemic and prevent future outbreaks in similar settings.
-
Target 3.d: Strengthen the capacity of all countries, in particular developing countries, for early warning, risk reduction and management of national and global health risks.
- The article serves as a risk assessment for dental clinics. It identifies weaknesses in current disinfection protocols and highlights the danger of transmission from asymptomatic patients. The recommendation to develop “practical and up-to-date disinfection procedures” is a direct call to strengthen risk management capacity in healthcare facilities.
SDG 6: Clean Water and Sanitation
-
Target 6.2: By 2030, achieve access to adequate and equitable sanitation and hygiene for all…
- The article’s analysis of disinfection protocols in dental clinics is directly related to this target. It questions the adequacy of current hygiene practices by showing that SARS-CoV-2 RNA was found on surfaces like the cuspidor and visor. The discussion about the ineffectiveness of certain disinfectants (quaternary ammonium compounds) against the virus and improper application methods (spraying) underscores the need for improved hygiene standards in institutional settings.
SDG 8: Decent Work and Economic Growth
-
Target 8.8: Protect labour rights and promote safe and secure working environments for all workers…
- The study’s primary motivation is the high risk of infection faced by dental professionals. The article mentions that “Dentists and allied healthcare personnel are in the high-risk group for bacterial and viral agents transmitted via aerosol.” By detecting viral RNA on protective equipment like gowns and visors, the study provides evidence of workplace hazards and implicitly advocates for better protective measures to ensure a safer working environment.
3. Are there any indicators mentioned or implied in the article that can be used to measure progress towards the identified targets?
SDG 3: Good Health and Well-being
- Indicator for Target 3.3: The prevalence of SARS-CoV-2. The article provides specific data points that serve as indicators: “SARS CoV-2 RNA positivity was observed in three (3%) patient samples and four (1.3%) environmental samples.” This quantifies the presence of the communicable disease in the studied population and environment.
- Indicator for Target 3.d: The effectiveness of health risk management protocols. The article implies this indicator by assessing the current disinfection procedures. The detection of viral RNA on surfaces after procedures (“one spittoon, and one visor”) serves as a negative indicator, showing that current risk management is insufficient.
SDG 6: Clean Water and Sanitation
- Indicator for Target 6.2: The level of surface contamination in a sanitized environment. The study measures this by testing for viral RNA on various surfaces. The finding of positive samples on the cuspidor, visor, and aprons is a direct indicator of the effectiveness (or lack thereof) of the hygiene and disinfection protocols in place.
SDG 8: Decent Work and Economic Growth
- Indicator for Target 8.8: The rate of occupational exposure to biological hazards. The article measures this by testing the personal protective equipment of dentists. The detection of SARS-CoV-2 on “two aprons… and one visor” is a direct indicator of the exposure risk faced by these workers, which is a measure of workplace safety. The article also cites external studies providing prevalence rates among dentists (“2.6%” and “3.7%”), which are established indicators for occupational health.
4. SDGs, Targets, and Indicators Table
| SDGs | Targets | Indicators Identified in the Article |
|---|---|---|
| SDG 3: Good Health and Well-being | 3.3: End epidemics and combat communicable diseases. |
|
| SDG 3: Good Health and Well-being | 3.d: Strengthen capacity for health risk management. |
|
| SDG 6: Clean Water and Sanitation | 6.2: Achieve access to adequate sanitation and hygiene for all. |
|
| SDG 8: Decent Work and Economic Growth | 8.8: Promote safe and secure working environments for all workers. |
|
Source: nature.com