Clinical Research Report: Paridiprubart for COVID-19 Respiratory Distress
Advancing Sustainable Development Goal 3: Good Health and Well-being
A recent clinical study indicates that the monoclonal antibody paridiprubart, when added to the standard of care (SOC), may significantly improve outcomes for Intensive Care Unit (ICU) patients with COVID-19-related respiratory distress. The findings, presented at the CHEST 2025 Annual Meeting, suggest a potential advancement in managing global health crises, directly supporting the objectives of SDG 3 by strengthening the capacity of health systems to manage severe communicable diseases.
Study Methodology and Global Collaboration
Objective and Design
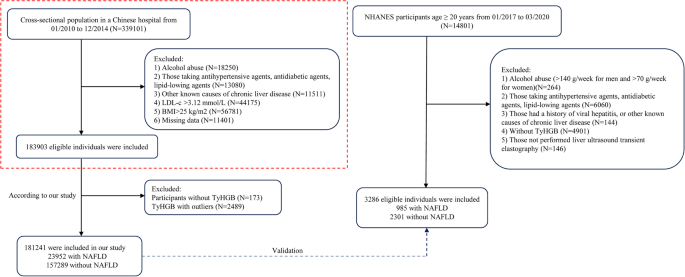
The Phase 3 study (NCT04401475) was designed to assess the efficacy of paridiprubart in improving disease severity among adults with respiratory failure. The primary objective was to measure the proportion of patients achieving a decrease of at least two points on the World Health Organization (WHO) COVID-19 Severity Scale (WCSS) by day 28. This research aligns with SDG 9 (Industry, Innovation, and Infrastructure) by investing in scientific research to develop novel health technologies.
Participant Cohort and Intervention
The trial demonstrates a commitment to SDG 17 (Partnerships for the Goals) through its international collaboration.
- Enrollment: 104 patients from 38 hospitals.
- Geographic Scope: Canada, Colombia, and the United States, reflecting a partnership to address health challenges that transcend borders and contribute to SDG 10 (Reduced Inequalities).
- Demographics: The mean age was 52 years, with 34% being women. All had laboratory-confirmed SARS-CoV-2 and required invasive mechanical ventilation (IMV).
- Randomization: Patients were assigned on a 1:1 basis to receive either paridiprubart plus SOC (n=56) or a placebo plus SOC (n=48).
Analysis of Clinical Outcomes
Primary Endpoint Achievement
The study successfully met its primary endpoint, demonstrating a clinically meaningful and statistically significant improvement in the paridiprubart group. These results are crucial for advancing SDG 3 by providing new tools to combat pandemics.
- Paridiprubart Group: An adjusted rate of 38% of patients achieved a WCSS score reduction of at least two points.
- Placebo Group: An adjusted rate of 27% of patients achieved the same reduction.
- Statistical Significance: The adjusted difference of 11% between the groups was statistically significant (P <.05).
A Cox regression analysis further suggested the paridiprubart group had a higher rate of achieving the primary outcome (Hazard Ratio [HR], 1.9), reinforcing the drug’s potential efficacy.
Implications for Sustainable Development Goals (SDGs)
Contribution to Health Systems and Economic Stability
The demonstrated efficacy of paridiprubart has significant implications for several SDGs by potentially accelerating clinical recovery and reducing the strain on critical healthcare resources.
- SDG 3 (Good Health and Well-being): By reducing patient dependence on invasive supportive measures and enabling earlier ICU discharge, the treatment can alleviate the burden on critical care infrastructure. This strengthens the overall resilience of health systems to manage current and future health emergencies.
- SDG 8 (Decent Work and Economic Growth): Faster patient recovery reduces the immense economic burden of prolonged critical illness on individuals, families, and national economies. A quicker return to health allows individuals to re-engage with the workforce, supporting economic productivity.
- SDG 10 (Reduced Inequalities): By potentially freeing up limited ICU beds, this therapeutic could improve equitable access to critical care for all patients, regardless of their condition, thereby addressing health inequalities.
Conclusion
The research on paridiprubart presents a promising therapeutic advancement for critically ill COVID-19 patients. The study authors concluded that its efficacy “suggests it could become an important therapeutic addition to the standard of care.” Beyond its immediate clinical benefits, the development and successful trial of this drug underscore the power of innovative, collaborative research in achieving the United Nations’ Sustainable Development Goals, particularly in building resilient health systems and fostering global well-being.
Analysis of Sustainable Development Goals in the Article
1. Which SDGs are addressed or connected to the issues highlighted in the article?
- SDG 3: Good Health and Well-being: The entire article is focused on this goal. It discusses a clinical trial for a new drug, paridiprubart, aimed at treating severe respiratory distress caused by COVID-19. The research seeks to improve health outcomes, accelerate clinical recovery, and enhance the standard of care for critically ill patients, which is central to ensuring healthy lives and promoting well-being for all at all ages.
2. What specific targets under those SDGs can be identified based on the article’s content?
- Target 3.3: End the epidemics of AIDS, tuberculosis, malaria and neglected tropical diseases and combat hepatitis, water-borne diseases and other communicable diseases. The article directly addresses this target by focusing on a treatment for COVID-19, a major communicable disease. The development of an effective therapeutic like paridiprubart is a crucial step in combating the pandemic and managing its impact on global health.
- Target 3.8: Achieve universal health coverage, including… access to quality essential health-care services and access to safe, effective, quality and affordable essential medicines… The research on paridiprubart aims to create a new, effective medicine. The article states that the drug “could become an important therapeutic addition to the standard of care,” directly contributing to the availability of quality essential medicines and improving the quality of health-care services for patients with severe COVID-19.
- Target 3.d: Strengthen the capacity of all countries… for early warning, risk reduction and management of national and global health risks. The article highlights that the new treatment could “reduce the burden on critical care resources.” By potentially reducing dependence on invasive mechanical ventilation and allowing for earlier discharge from the ICU, the drug strengthens the capacity of healthcare systems to manage the surge of patients during a global health crisis like the COVID-19 pandemic. The study’s inclusion of hospitals in Canada, Colombia, and the United States also points to strengthening this capacity across different countries.
3. Are there any indicators mentioned or implied in the article that can be used to measure progress towards the identified targets?
- Yes, the article mentions and implies several specific indicators:
- Reduction in disease severity score: The primary outcome of the study was explicitly defined as “the proportion of patients with a decrease of at least 2 points in the World Health Organization (WHO) COVID-19 Severity Scale (WCSS) score at 28 days.” This serves as a direct, measurable indicator of improved health outcomes and the efficacy of the new treatment.
- Rate of clinical recovery: The article mentions that the drug could “accelerate clinical recovery.” The Cox regression analysis, which showed an “88% higher rate for paridiprubart vs placebo in achieving a WCSS reduction,” is a statistical measure of this accelerated recovery rate.
- Reduced dependence on critical care resources: The article implies indicators related to healthcare system capacity. It states the treatment may “reduce dependence on invasive supportive measures” (like invasive mechanical ventilation) and “allow earlier discharge.” These outcomes are measurable indicators of a reduced burden on ICUs and other critical care resources.
4. Table of SDGs, Targets, and Indicators
| SDGs | Targets | Indicators |
|---|---|---|
| SDG 3: Good Health and Well-being | 3.3: Combat communicable diseases. |
|
| SDG 3: Good Health and Well-being | 3.8: Access to quality essential health-care services and effective medicines. |
|
| SDG 3: Good Health and Well-being | 3.d: Strengthen capacity for management of global health risks. |
|
Source: pulmonologyadvisor.com