Post-COVID-19 Health Complications and Sustainable Development Goal 3
Introduction
The management of severe COVID-19 has presented significant challenges to global health systems, impacting the achievement of Sustainable Development Goal 3 (SDG 3), which aims to ensure healthy lives and promote well-being for all at all ages. A notable complication is the emergence of opportunistic infections, such as Endogenous Endophthalmitis (EE), in patients who have undergone treatment for severe COVID-19. This report examines the factors contributing to this condition, the diagnostic and therapeutic challenges, and the implications for health equity, framing the discussion within the context of the SDGs.
Diagnostic Challenges and Implications for Universal Health Coverage (SDG 3.8)
Immunological Predisposition in Post-COVID-19 Patients
An impaired immunologic response in patients with severe COVID-19 creates a predisposition to opportunistic infections, undermining efforts to provide quality healthcare as outlined in SDG 3. Key contributing factors include:
- High and/or prolonged doses of corticosteroids.
- Prolonged hospitalization periods.
- Use of immunosuppressive drugs.
- COVID-19 viremia leading to a decrease in peripheral lymphocytes.
The lack of standardized clinical protocols for corticosteroid use during the pandemic resulted in significant treatment variability and potential overuse. This inconsistency highlights a gap in ensuring equitable and quality healthcare, a core target of SDG 3.
Microbiological Diagnostic Difficulties
Effective diagnosis is fundamental to universal health coverage (Target 3.8). However, diagnosing EE presents considerable challenges:
- Obtaining positive cultures in EE is rare. Case series in India reported no exact microbiological diagnosis even with vitreous biopsy.
- Large-scale studies report positive cultures from ocular fluids in only 14–43% of EE cases.
- Despite negative blood cultures, Candidemia (especially from C. albicans) is frequently the underlying cause.
- Ocular manifestations can be the first sign of candidemia, making prompt diagnosis critical to reducing complications and aligning with the goal of effective health services.
Treatment Outcomes and the Pursuit of Well-being (SDG 3)
Visual Prognosis and Health Outcomes
The visual outcomes in EE are generally poor, posing a significant threat to patient well-being and quality of life, a central concern of SDG 3.
- Visual Acuity (VA) in EE cases can range from 6/6 to no perception of light (NPL).
- Bacterial EE, particularly from Klebsiella species, often results in worse outcomes than endogenous fungal endophthalmitis (EFE).
- Among fungal causes, Aspergillus has a worse prognosis than C. albicans.
- Treatment with voriconazole for Candida endophthalmitis has shown VA outcomes ranging from 20/20 to 20/100 in survivors.
Importance of Timely Intervention
Achieving good health outcomes depends on responsive and timely medical intervention. Reports indicate that good visual outcomes are achievable in EFE when timely diagnosis and treatment are initiated, reinforcing the importance of strengthening health systems to meet the targets of SDG 3.
Therapeutic Strategies and Healthcare Inequalities (SDG 3 & SDG 10)
Recommended Treatment Modalities
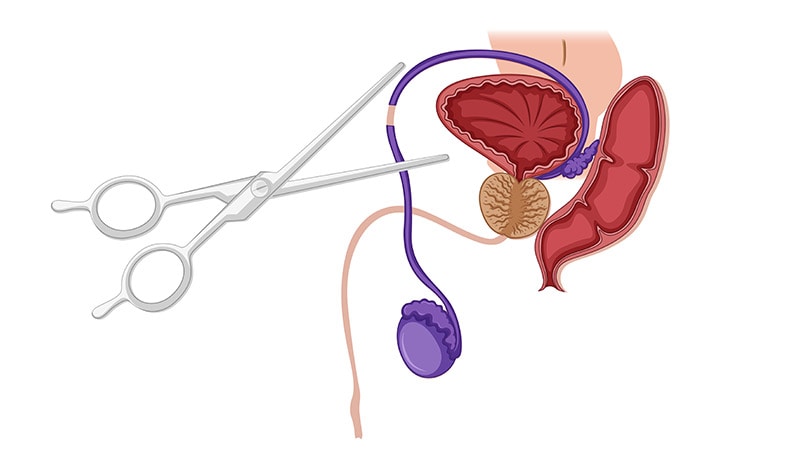
An effective therapeutic strategy is crucial for managing EFE and ensuring patient health. The optimal approach combines several modalities:
- Vitrectomy, especially in cases of severe vitritis.
- Intravitreal injection of an antifungal agent, such as amphotericin B or voriconazole.
- Systemic antifungal therapy, including agents like voriconazole or fluconazole.
Barriers to Access and Health Inequity (SDG 10)
Disparities in access to essential medicines undermine SDG 10 (Reduced Inequalities) and SDG 3. The situation in Venezuela exemplifies this challenge:
- Access to amphotericin B, a key antifungal agent, is extremely limited and its supply is inconsistent.
- This inequality forces reliance on more readily available alternatives like voriconazole, highlighting how geographic and economic factors dictate the quality of care.
Such disparities create significant barriers to achieving universal health coverage and ensuring that all individuals receive the care they need.
Conclusion: Strengthening Health Systems for Sustainable Development
Recommendations for Aligning with SDG 3
This analysis underscores the need for a robust and equitable healthcare response to post-pandemic complications. To better align with the principles of SDG 3 and SDG 10, the following actions are imperative:
- Maintain a high index of suspicion for EE in post-COVID-19 patients, particularly those with comorbidities like diabetes and a history of corticosteroid use.
- Promote prompt ophthalmic cross-consultation to facilitate early diagnosis and timely intervention, preventing severe vision-related complications.
- Develop and implement standardized clinical guidelines for managing post-COVID-19 complications to ensure consistent and high-quality care for all patients.
- Address global disparities in access to essential medicines to reduce health inequalities and move closer to the goal of universal health coverage.
Analysis of Sustainable Development Goals in the Article
1. Which SDGs are addressed or connected to the issues highlighted in the article?
-
SDG 3: Good Health and Well-being
This is the most central SDG in the article. The entire text focuses on a specific health crisis: the emergence of opportunistic fungal infections (endogenous endophthalmitis – EE) as a severe complication of COVID-19 treatment. It discusses disease pathology, diagnosis, treatment protocols, patient outcomes (visual acuity), and access to essential medicines, all of which are core components of ensuring healthy lives and promoting well-being.
-
SDG 10: Reduced Inequalities
The article implicitly addresses this goal by highlighting disparities in healthcare access. It specifically mentions that in Venezuela, “access to amphotericin B—particularly for intravitreal use—is extremely limited, and its supply is inconsistent.” This points to inequalities in the availability of essential medicines between different regions, which can lead to unequal health outcomes for patients with the same condition.
-
SDG 16: Peace, Justice and Strong Institutions
This goal is relevant through the article’s critique of institutional responses during the COVID-19 pandemic. The text states that the “use of corticosteroids during the COVID-19 pandemic was neither standardized nor guided by clear clinical protocols, which resulted in significant variability, and at times, overuse.” This lack of definitive guidelines from health institutions points to a weakness in developing effective and accountable institutional processes during a global health emergency.
2. What specific targets under those SDGs can be identified based on the article’s content?
-
SDG 3: Good Health and Well-being
- Target 3.3: “By 2030, end the epidemics of AIDS, tuberculosis, malaria and neglected tropical diseases and combat hepatitis, water-borne diseases and other communicable diseases.” The article directly addresses this target by focusing on managing a severe complication (fungal EE) arising from a communicable disease (COVID-19). The discussion on diagnosing and treating these opportunistic infections is central to combating the overall impact of the pandemic.
- Target 3.8: “Achieve universal health coverage, including financial risk protection, access to quality essential health-care services and access to safe, effective, quality and affordable essential medicines and vaccines for all.” The article highlights the challenge of accessing essential medicines by noting the limited availability of amphotericin B in Venezuela. It also discusses the importance of quality healthcare services, such as “prompt ophthalmic cross-consultation” and timely interventions like vitrectomy, to achieve good visual outcomes.
- Target 3.d: “Strengthen the capacity of all countries, in particular developing countries, for early warning, risk reduction and management of national and global health risks.” The article underscores the need to strengthen the management of health risks associated with the pandemic. It calls for a “high index of suspicion for EE in patients with COVID-19” and emphasizes that the lack of standardized protocols for corticosteroid use represents a gap in risk management capacity.
-
SDG 10: Reduced Inequalities
- Target 10.3: “Ensure equal opportunity and reduce inequalities of outcome…” The limited access to a first-line treatment (amphotericin B) in a specific region (Venezuela) directly contributes to potential inequalities in health outcomes. Patients in this region may have to rely on alternative treatments, which could affect their prognosis compared to patients in better-supplied regions.
-
SDG 16: Peace, Justice and Strong Institutions
- Target 16.6: “Develop effective, accountable and transparent institutions at all levels.” The article’s observation that corticosteroid use was “neither standardized nor guided by clear clinical protocols” during the pandemic serves as a direct critique of the effectiveness of health institutions in providing clear and consistent guidance, which is a key aspect of this target.
3. Are there any indicators mentioned or implied in the article that can be used to measure progress towards the identified targets?
-
Indicators for SDG 3
- Incidence of opportunistic infections post-pandemic: The article’s focus on case series of fungal EE post-COVID-19 in India and the identification of specific pathogens like Candida and Aspergillus imply that tracking the incidence of such complications is a key measure of how well communicable diseases are being managed (relevant to Target 3.3).
- Availability of essential medicines: The explicit statement that “access to amphotericin B… is extremely limited” in Venezuela serves as a direct, qualitative indicator for measuring access to affordable essential medicines (relevant to Target 3.8).
- Patient health outcomes: The article frequently mentions Visual Acuity (VA) outcomes, citing ranges “from Snell 6/6 to no perception of light (NPL).” This is a specific clinical indicator that can measure the quality and effectiveness of healthcare services provided (relevant to Target 3.8).
-
Indicators for SDG 10
- Geographic disparities in drug availability: The contrast between the limited supply of amphotericin B in Venezuela and the availability of an alternative (voriconazole) is an implied indicator of regional inequalities in healthcare resources (relevant to Target 10.3).
-
Indicators for SDG 16
- Existence and application of standardized clinical protocols: The article’s direct statement about the absence of “definitive guidelines” or “clear clinical protocols” for corticosteroid use during the pandemic can be used as a qualitative indicator to assess the effectiveness and accountability of health institutions (relevant to Target 16.6).
4. Summary Table of SDGs, Targets, and Indicators
| SDGs | Targets | Indicators Identified in the Article |
|---|---|---|
| SDG 3: Good Health and Well-being |
3.3: Combat communicable diseases.
3.8: Achieve universal health coverage and access to essential medicines. 3.d: Strengthen capacity for health risk management. |
– Incidence of opportunistic infections (fungal EE) following a communicable disease (COVID-19).
– Availability of essential medicines (e.g., limited access to amphotericin B in Venezuela). – The stated absence of standardized clinical protocols for corticosteroid use during the pandemic. |
| SDG 10: Reduced Inequalities | 10.3: Ensure equal opportunity and reduce inequalities of outcome. | – Geographic disparities in the availability of essential drugs (amphotericin B being limited in Venezuela). |
| SDG 16: Peace, Justice and Strong Institutions | 16.6: Develop effective, accountable and transparent institutions at all levels. | – Lack of “standardized” or “clear clinical protocols” from health institutions for managing COVID-19 treatments. |
Source: jmedicalcasereports.biomedcentral.com